Researchers say they have reported the first results demonstrating clinical activity of a CD22-directed chimeric antigen receptor (CAR) T-cell therapy in B-cell acute lymphoblastic leukemia (B-ALL).
The team conducted a phase 1 study of the therapy in 21 children and adults with relapsed/refractory B-ALL.
Twelve patients achieved a complete response (CR) to the treatment, with 3 patients still in CR at last follow-up.
Sixteen patients developed cytokine release syndrome (CRS), all grade 1 or 2.
Crystal Mackall, MD, of Stanford University in California, and her colleagues reported these results in Nature Medicine.*
“This is the first time that we’ve seen response rates anything like we achieved when we were first testing the CD19 CAR T therapy,” Dr Mackall said.
“We were all a little worried that we wouldn’t find anything comparable, but this study gives hope to the idea that there may be another similar, very potent treatment.”
Patients
Dr Mackall and her colleagues studied the CD22-CAR T-cell therapy in 21 patients with relapsed/refractory B-ALL. They had a median age of 19 (range, 7 to 30).
All of the patients had received a hematopoietic stem cell transplant at least once, and 2 patients had 2 prior transplants each. Seventeen patients had received prior CD19-directed immunotherapy. Fifteen had received CD19-directed CAR T-cell therapy, and 2 had received blinatumomab.
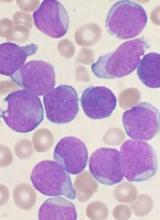
Lymphoblasts were CD19− or CD19dim in 10 patients (9 who had received a CD19-CAR and 1 treated with blinatumomab).
The median CD22 site density was 2839 molecules per cell (range, 613 to 13,452).
Dosing and DLTs
Patients received the CD22-CAR T-cell therapy at 1 of 3 dose levels:
- 0.3 × 106 CD22-CAR T cells per kg body weight (n=6)
- 1 × 106 cells per kg (n=13)
- 3 × 106 cells per kg (n=2).
There was 1 dose-limiting toxicity (DLT) at the first dose level. It was grade 3, self-limited, noninfectious diarrhea that occurred during CRS and resolved with supportive care.
The other DLT occurred in a patient who received treatment at the third dose level. This patient had grade 4 hypoxia that was associated with rapid disease progression. The patient required brief intubation, and the hypoxia was resolved within 24 hours of starting steroid treatment.
Based on these results, the second dose level became the recommended phase 2 dose.
Other adverse events
The researchers said the primary toxicity was CRS, which occurred in 16 patients. Nine patients had grade 1 CRS, and 7 had grade 2.
There were no cases of irreversible neurotoxicity or seizure reported. Among the first 16 patients with complete assessments, there were cases of transient visual hallucinations (n=2), mild unresponsiveness (n=1), mild disorientation (n=1), and mild to moderate pain (n=2). However, these incidents resolved by day 28.
One patient died from gram-negative rod sepsis that developed after the resolution of CRS and neutrophil count recovery to >1000 cells/μL blood. The patient had a history of multi-organ failure due to sepsis.
Response
Twelve patients (57%) had a CR, and 9 of them were minimal residual disease negative.
One CR occurred at the lowest dose of therapy, 1 occurred at the highest dose, and the remaining 10 CRs occurred in patients who received dose level 2.
The researchers said there was no evidence to suggest that previous CD19-directed immunotherapy or diminished surface expression of CD19 impacted response to the CD22-CAR T-cell therapy.
Of the 9 patients who did not respond, 4 progressed and 5 had stable disease.
The researchers said 4 non-responders had “very high disease burden with rapid disease progression.” And 2 non-responders expressed diminished or partial CD22 on leukemic blasts at the time of enrollment.
The median duration of response was 6 months (range, 1.5 to 21+ months). Three patients are still in CR at 6, 9, and 21 months of follow-up.
“The take-home message is that we’ve found another CAR T-cell therapy that displays high-level activity in this phase 1 trial,” Dr Mackall said. “But the relapse rate was also high. So this forces the field to get even more sophisticated. How much of a target is needed for successful, long-lasting treatment? What happens if we target both CD19 and CD22 simultaneously?”
The researchers are already tackling the last question by testing a CAR T-cell therapy that recognizes both CD19 and CD22. They’ve confirmed this therapy can kill cancer cells in vitro and in vivo. Now, they’re testing it in a clinical trial that has opened at Stanford University and will open soon at the National Cancer Institute.
*This research was supported, in part, by the Intramural Research Program, National Cancer Institute and NIH Clinical Center, National Institutes of Health; by a Stand Up to Cancer–St. Baldrick’s Pediatric Dream Team translational research grant; and by a St. Baldrick’s Foundation Scholar Award.