MAINZ/FRANKFURT, GERMANY—Outcomes of treatment with a third-generation chimeric antigen receptor (CAR) T-cell therapy are associated with a patient’s immune status, according to a phase 1/2a trial.
The CD19-specific CAR T-cell therapy produced a complete response (CR) in 6 of 15 patients with relapsed/refractory CD19-positive leukemia or lymphoma.
Though all responders eventually relapsed, 4 patients—including 2 with stable disease (SD) after treatment—responded to subsequent therapy and are still alive, 1 of them beyond 36 months.
An analysis of blood samples taken throughout the study revealed that a patient’s immune status was associated with treatment failure and overall survival.
Tanja Lövgren, PhD, of Uppsala University in Sweden, and her colleagues presented these findings at the Third CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference: Translating Science into Survival (abstract B156).
“CD19-specific CAR T-cell therapy has yielded remarkable response rates for patients who have B-cell acute lymphoblastic leukemia,” Dr Lövgren said. “However, many patients relapse.”
“In addition, response rates are more variable for patients who have other CD19-positive B-cell malignancies, and many patients experience serious adverse events. We set out to investigate the safety and effectiveness of a third-generation CD19-specific CAR T-cell therapy and to identify potential biomarkers of treatment outcome.”
Dr Lövgren and her colleagues studied 15 patients (ages 24-72) who had relapsed or refractory CD19-positive B-cell malignancies:
- Six patients with diffuse large B-cell lymphoma (DLBCL), including 3 cases that were transformed from follicular lymphoma (FL)
- Four patients with pre-B acute lymphoblastic leukemia (ALL)
- Two patients with mantle cell lymphoma (MCL)
- Two patients with chronic lymphocytic leukemia (CLL)
- One patient with FL transformed from Burkitt lymphoma.
Eleven patients received preconditioning with cyclophosphamide (500 mg/m2) and fludarabine (3 doses at 25 mg/m2).
All patients received CAR T cells at 1 x 108, 2 x 107, or 2 x 108 cells/m2. These were autologous, CD19-targeting CAR T cells with 3 intracellular signaling domains derived from CD3 zeta, CD28, and 4-1BB.
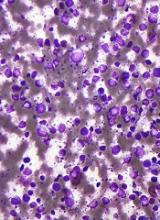
The researchers assessed tumor responses via bone marrow/blood analysis and/or radiology, depending on the type of malignancy. The team also collected blood samples before CAR T-cell infusion and at multiple times after infusion.
Efficacy and safety
Six patients achieved a CR to treatment—3 with DLBCL (1 transformed), 2 with ALL, and 1 with CLL. Two patients had SD—1 with MCL and 1 with CLL. The remaining patients progressed.
All patients with a CR eventually relapsed. The median duration of CR was 5 months (range, 3-24 months).
Four patients—2 complete responders and 2 with SD—responded well to subsequent therapy and are still alive with 27 to 36 months of follow-up. This includes 1 patient with DLBCL, 1 with MCL, and 2 with CLL.
Four patients had serious adverse events. Three had cytokine-release syndrome, and 2 had neurological toxicity.
All cases of cytokine-release syndrome resolved after treatment with corticosteroids/anti-IL6R therapy. The neurological toxicity resolved spontaneously.
Immune status
An analysis of the blood samples taken throughout the study showed that high levels of monocytic myeloid-derived suppressor cells (MDSCs) prior to treatment was associated with decreased overall survival. In addition, increased levels of MDSCs after treatment preceded treatment failure.
Furthermore, high plasma levels of immunosuppressive factors—such as PD-L1 and PD-L2—after treatment were associated with decreased overall survival.
High plasma levels of biomarkers of an immunostimulatory environment—including IL-12, DC-LAMP, TRAIL, and FasL—before the administration of CAR T-cell therapy was associated with increased overall survival.
“[A]n immunostimulatory environment was associated with improved overall survival, while immunosuppressive cells and factors were associated with treatment failure and decreased overall survival,” Dr Lövgren said.
“We are hoping to follow up this study with another clinical trial that will combine CAR T-cell therapy with chemotherapy known to decrease the number of monocytic myeloid-derived suppressive cells. We are also looking to further optimize the CAR T-cell therapy.”
Dr Lövgren said the main limitations of this study are that it only included 15 patients, the patients had several different malignancies, and some patients may have been too sick to respond to any treatment.
This study was supported by funds from AFA Insurance AB, the Swedish Cancer Society, the Swedish Research Council, the Lions Fund at Uppsala University Hospital, and the Swedish State Support for Clinical Research. Dr Lövgren declared no conflicts of interest.