The US Food and Drug Administration (FDA) has granted priority review to a supplemental new drug application (sNDA) for the tyrosine kinase inhibitor (TKI) bosutinib (Bosulif®).
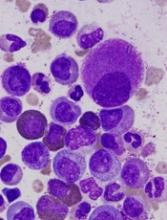
If approved, the sNDA would expand the use of bosutinib to include patients with newly diagnosed, chronic phase, Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML).
Bosutinib is currently FDA-approved to treat adults with chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to prior therapy.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency’s goal is to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA plans to make a decision on the sNDA for bosutinib by the end of this year.
Meanwhile, the European Medicines Agency (EMA) has validated for review a type II variation application for bosutinib in patients with newly diagnosed, chronic phase Ph+ CML.
Bosutinib already has conditional marketing authorization in the European Economic Area for the treatment of adults with Ph+ CML who previously received at least 1 TKI and adults with Ph+ CML for whom imatinib, nilotinib, and dasatinib are not considered appropriate.
Phase 3 trial
The applications submitted to the EMA and FDA are both supported by early results from the phase 3 BFORE trial. Results from this trial were presented at the ASCO Annual Meeting in May.
In this ongoing study, researchers are comparing bosutinib and imatinib as first-line treatment of chronic phase CML.
As of the ASCO presentation, the trial had enrolled 536 patients who were randomized 1:1 to receive bosutinib (n=268) or imatinib (n=268).
The presentation included results in a modified intent-to-treat population of Ph+ patients with e13a2/e14a2 transcripts who had at least 12 months of follow-up. In this group, there were 246 patients in the bosutinib arm and 241 in the imatinib arm.
Most of the patients were still on therapy at the 12-month mark or beyond—78% in the bosutinib arm and 73.2% in the imatinib arm. The median treatment duration was 14.1 months and 13.8 months, respectively.
At 12 months, the rate of major molecular response was 47.2% in the bosutinib arm and 36.9% in the imatinib arm (P= 0.02). The rate of complete cytogenetic response was 77.2% and 66.4%, respectively (P<0.008).
One patient in the bosutinib arm and 4 in the imatinib arm discontinued treatment due to disease progression, while 12.7% and 8.7%, respectively, discontinued treatment due to drug-related toxicity.
Adverse events that were more common in the bosutinib arm than the imatinib arm included grade 3 or higher diarrhea (7.8% vs 0.8%), increased alanine levels (19% vs 1.5%), increased aspartate levels (9.7% vs 1.9%), cardiovascular events (3% vs 0.4%), and peripheral vascular events (1.5% vs 1.1%). Cerebrovascular events were more common with imatinib than bosutinib (0.4% and 0%, respectively).