A 3-arm phase 2 study of azacitidine alone or in combination with lenalidomide or vorinostat in patients with higher-risk myelodysplastic syndromes (MDS) or chronic myelomonocytic leukemia (CMML) has shown the combination therapies to have similar overall response rates (ORR) to azacitidine monotherapy. Based on these findings, investigators did not choose either combination arm for phase 3 testing of overall survival.
However, patients with CMML treated with the azacitidine-lenalidomide combination had twice the ORR compared with azacitidine monotherapy, they reported.
And patients with certain mutations, such as DNMT3A, BCOR, and NRAS, had higher overall response rates, although only those with the DNMT3A mutation were significant.
Mikkael A. Sekeres, MD, of the Cleveland Clinic in Cleveland, Ohio, and colleagues reported these findings in the Journal of Clinical Oncology on behalf of the North American Intergroup Study SWOG S117.
Doses of azacitidine were the same for monotherapy and combination arms: 75 mg/m2/day intravenously or subcutaneously on days 1 to 7 of a 28-day cycle.
Patients in the lenalidomide arm received 10 mg/day orally of that drug on days 1 to 21, and patients in the vorinostat arm received 300 mg twice daily orally on days 3 to 9.
Patient characteristics
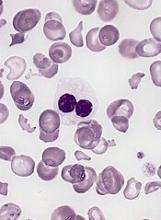
Patients had MDS of IPSS Intermediate-2 or higher or bone marrow blasts 5% or greater. Patients with CMML had fewer than 20% blasts.
The investigators randomized 277 patients to receive either azacitidine alone (n=92), azacitidine plus lenalidomide (n=93), or azacitidine plus vorinostat (n=92).
Patients were a median age of 70 years (range, 28 to 93). Eighty-five patients (31%) were female, 53 (19%) had CMML, and 18 (6%) had treatment-related MDS. More than half the patients were transfusion-dependent at baseline.
Baseline characteristics were similar across the 3 arms. The investigators noted that the baseline characteristics were also similar across the 90 centers participating in the study, whether they were an MDS Center of Excellence or a high-volume center.
Adverse events
For the most part, therapy-related adverse events were similar across the arms.
Rates of grade 3 or higher febrile neutropenia and infection and infestations were similar for all 3 cohorts: 89% for azaciditine monotherapy, 91% for the lenalidomide combination, and 91% for the vorinostat combination.
However, the vorinostat arm had more grade 3 or higher gastrointestinal toxicities (14 patients, 15%) compared with the monotherapy arm (4 patients, 4%), P=0.02.
And patients receiving lenalidomide experienced more grade 3 or higher rash (14 patients, 16%) compared with patients receiving monotherapy (3 patients, 3%), P=0.005.
Patients in the combination arms stopped therapy at significantly higher rates than the monotherapy arm. Eight percent of patients receiving monotherapy stopped treatment compared with 20% in the lenalidomide arm and 21% in the vorinostat arm.
Patients in the combination arms also had more dose modifications not specified in the protocol than those in the monotherapy arm. Twenty-four percent receiving azacitidine monotherapy had non-protocol defined dose modifications, compared with 43% in the lenalidomide arm and 42% in the vorinostat arm.
Responses
The ORR for the entire study population was 38%.
Patients in the monotherapy arm had an ORR of 38%, those in the lenalidomide arm, 49%, and those in the vorinostate arm, 27%. Neither arm achieved significance compared with the monotherapy arm.
Patients who were treatment-naïve in the lenalidomide arm had a somewhat improved ORR compared with monotherapy, P=0.08.
The median duration of response for all cohorts was 15 months: 10 months for monotherapy, 14 months for lenalidomide, and 18 months for vorinostat.
Patients who were able to remain on therapy for 6 months or more in the lenalidomide arm achieved a higher ORR of 87% compared with monotherapy (62%, P=0.01). However, there was no difference in response duration with longer therapy.
The median overall survival (OS) was 17 months for all patients, 15 months for patients in the monotherapy group, 19 months for those in the lenalidomide arm, and 17 months for those in the vorinostat group.
CMML patients had similar OS across treatment arms, with the median not yet reached for patients in the monotherapy arm.
Subgroup responses
Patients with CMML in the lenalidomide arm had a significantly higher ORR than CMML patients in the monotherapy arm, 68% and 28%, respectively (P=0.02).
Median duration of response for CMML patients was 19 months, with no differences between the arms.
The investigators observed no differences in ORR for therapy-related MDS, IPSS subgroups, transfusion-dependent patients, or allogeneic transplant rates.
However, they noted ORR was better for patients with chromosome 5 abnormality regardless of treatment arm than for those without the abnormality (odds ratio, 2.17, P=0.008).
One hundred thirteen patients had mutational data available. They had a median number of 2 mutations (range, 0 to 7), with the most common being ASXL1 (n = 31), TET2 (n = 26), SRSF2 (n = 23), TP53 (n = 22), RUNX1 (n = 21), and U2AF1 (n = 19).
Patients with DNMT3A mutation had a significantly higher ORR than for patients without mutations, 67% and 34%, respectively P=0.025).
Patients with BCOR and NRAS mutations had numerically higher, but non-significant, ORR than non-mutated patients. Patients with BCOR mutation had a 57% ORR compared with 34% for non-mutated patients (P=0.23). Patients with NRAS mutation had a 60% ORR compared with 36% for non-mutated patients (P=0.28).
Patients with mutations in TET2 (P = .046) and TP53 (P = .003) had a worse response duration than those without mutations.
Response duration was significantly better with fewer mutations. For 2 or more mutations, the hazard ration was 6.86 versus no mutations (P=0.01).
The investigators believed under-dosing may have compromised response and survival in the combination arms. They suggested that studies focused on the subgroups that seemed to benefit from the combinations should be conducted.