A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
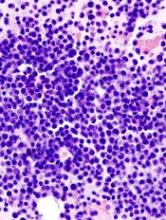
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.