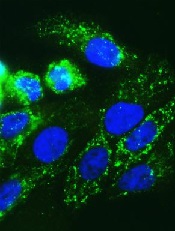
Credit: Juha Klefstrom
New research indicates that an unexpected partnership between the MYC oncogene and a non-coding RNA called PVT1 could be the key to understanding how MYC fuels cancers.
The researchers knew that MYC amplifications cause cancer, but MYC does not amplify alone. It often pairs with adjacent chromosomal regions.
“We wanted to know if the neighboring genes played a role,” said study author Anindya Bagchi, PhD, of the University of Minnesota in Minneapolis.
“We took a chance and were surprised to find this unexpected and counter-intuitive partnership between MYC and its neighbor, PVT1. Not only do these genes amplify together, PVT1 helps boost the MYC protein’s ability to carry out its dangerous activities in the cell.”
The researchers reported this finding in Nature.
Dr Bagchi and his team focused on a region of the genome, 8q24, which contains the MYC gene and is commonly expressed in cancer. The team separated MYC from the neighboring region containing the non-coding RNA PVT1.
Using chromosome engineering, the researchers developed mouse strains in 3 separate iterations: MYC only, the rest of the region containing PVT1 but without MYC, and the pairing of MYC with the regional genes.
The expected outcome, if MYC was the sole driver of the cancer, was tumor growth on the MYC line as well as the paired line. However, the researchers found growth only on the paired line. This suggests MYC is not acting alone and needs help from adjacent genes.
“The discovery of this partnership gives us a stronger understanding of how MYC amplification is fueled,” said David Largaespada, PhD, also of the University of Minnesota.
“When cancer promotes a cell to make more MYC, it also increases the PVT1 in the cell, which, in turn, boosts the amount of MYC. It’s a cycle, and now we’ve identified it, we can look for ways to uncouple this dangerous partnership.”
Testing this theory of uncoupling, the researchers looked closely at several breast and colorectal cancers that are driven by MYC. For example, in colorectal cancer lab models, where a mutation in the beta-catenin gene drives MYC to cancerous levels, eliminating PVT1 from these cells made the tumors nearly disappear.
“Finding the cooperation between MYC and PVT1 could be a game changer,” said Yuen-Yi Tseng, a graduate student at the University of Minnesota.
“We used to think MYC amplification is the major issue but ignored that other co-amplified genes, such as PVT1, can be significant. In this study, we show that PVT1 can be a key regulator of MYC protein, which can shift the paradigm in our understanding of MYC-amplified cancers.”
MYC has been notoriously elusive as a drug target. By uncoupling MYC and PVT1, the researchers suspect they could disable the cancer growth and limit MYC to precancerous levels. This would make PVT1 an ideal drug target to potentially control a major cancer gene.
“This is a thrilling discovery, but there are more questions that follow,” Dr Bagchi said. “Two major areas present themselves now for research. Will breaking the nexus between MYC and PVT1 perform the same in any MYC-driven cancer, even those not driven by this specific genetic location?”
“And how is PVT1 stabilizing or boosting MYC within the cells? This relationship will be a key to developing any drugs to target this mechanism.”

