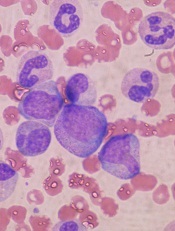
in the bone marrow
Hematopoietic stem cells (HSCs) require a highly regulated rate of protein synthesis to function properly, according to research published in Nature.
Experiments showed that a ribosomal mutation decreases protein synthesis in HSCs, and deletion of a tumor suppressor gene increases protein synthesis.
But both changes result in impaired HSC function.
In mouse models, the mutation counteracted the effects of the deletion, which restored normal HSC function and delayed leukemogenesis.
“We unveiled new areas of cellular biology that no one has seen before,” said study author Sean Morrison, PhD, of the University of Texas Southwestern Medical Center in Dallas.
“This finding not only tells us something new about stem cell regulation but opens up the ability to study differences in protein synthesis between many kinds of cells in the body. We believe there is an undiscovered world of biology that allows different kinds of cells to synthesize protein at different rates and in different ways, and that those differences are important for cellular survival.”
In a previous study, researchers discovered that, by modifying the antibiotic puromycin, they could measure protein synthesis in rare cells in vivo.
Dr Morrison and his colleagues realized they could adapt this reagent to measure protein synthesis in HSCs and other cells in the hematopoietic system.
Their analyses showed that different types of blood cells produced vastly different amounts of protein per hour. And HSCs, in particular, synthesized much less protein than other hematopoietic progenitors.
“This result suggests that blood-forming stem cells require a lower rate of protein synthesis as compared to other blood-forming cells,” Dr Morrison said.
He and his colleagues then generated mice with a mutation in a component of the ribosome (Rpl24Bst/+ mice). HSCs in these mice had a 30% lower rate of protein production than controls.
The researchers observed the opposite effect when they deleted the tumor suppressor gene Pten in mouse HSCs. These mice saw a roughly 30% increase in protein production relative to controls.
However, as in the Rpl24Bst/+ mice, HSC function was noticeably impaired in these animals.
Together, these observations suggest that HSCs require a highly regulated rate of protein synthesis, such that increases or decreases in that rate impair HSC function.
“Amazingly, when the ribosomal mutant mice and the Pten mutant mice were bred together, stem cell function returned to normal, and we greatly delayed, and in some instances entirely blocked, the development of leukemia,” Dr Morrison said.
“All of this happened because protein production in stem cells was returned to normal. It was as if two wrongs made a right.”

