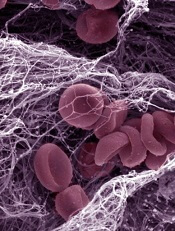
Credit: Kevin MacKenzie
Updated guidelines from the American Academy of Neurology provide a comparison of oral anticoagulants as stroke prophylaxis in patients with nonvalvular atrial fibrillation (NVAF).
The guidelines suggest that newer anticoagulants, such as dabigatran, rivaroxaban, and apixaban, are at least as effective, if not more effective, than warfarin at preventing stroke in patients with NVAF. But bleeding risks vary.
Clopidogrel plus aspirin appears to be less effective than warfarin and its derivatives but more effective than aspirin alone.
Apixaban also appears to be more effective than aspirin, with a similar bleeding risk. And triflusal plus acenocoumarol is likely more effective than acenocoumarol alone.
“Of course, doctors will need to consider the individual patient’s situation in making a decision whether or not to use anticoagulants and which one to use, as the risks and benefits can vary for each person,” said guideline author Antonio Culebras, MD, of SUNY Upstate Medical University in Syracuse, New York.
Comparing therapies
The authors noted that several new anticoagulants have been developed since the American Academy of Neurology’s last published guidelines on this topic, in 1998.
For the current guidelines, the authors evaluated the results of 6 studies comparing antithrombotics to warfarin and its derivatives, as well as 2 studies comparing antithrombotics to aspirin.
One study suggested that dabigatran is probably more effective than warfarin for reducing the risk of stroke or systemic embolism. Hemorrhage risks were similar with the 2 drugs. But intracranial hemorrhage was less frequent with dabigatran, and gastrointestinal bleeding was higher with dabigatran.
Another study indicated that rivaroxaban is likely as effective as warfarin for preventing cerebral and systemic embolism. Patients who received rivaroxaban had an increased risk of gastrointestinal bleeding but a decreased risk of intracranial hemorrhage and fatal bleeding.
Apixaban seemed to be more effective than warfarin in patients with NVAF who were at moderate risk of embolism. However, this superiority appeared to be the result of a decreased risk in bleeding and reduced mortality. Apixaban was no more effective than warfarin in reducing the risk of cerebral and systemic embolism.
Yet another study suggested that vitamin K antagonists (VKAs) are likely more effective than clopidogrel plus aspirin as stroke prevention in NVAF patients. However, intracranial bleeding was more common with VKAs.
In NVAF patients at moderate risk of stroke, treatment with triflusal plus acenocoumarol and moderate-intensity anticoagulation (INR target 1.25–2.0) appeared to be more effective than treatment with acenocoumarol alone and conventional-intensity anticoagulation (INR target 2.0–3.0).
Low-dose aspirin plus dose-adjusted VKA (fluindione) appeared to increase the risk of hemorrhagic complications compared to VKA therapy alone. However, there was not enough evidence to determine whether aspirin plus VKA decreases the risk of ischemic stroke or other thromboembolic events.
Apixaban appeared to be more effective than aspirin for decreasing the risk of stroke or systemic embolism in patients with NVAF who have a moderate risk of embolism and are not candidates for warfarin treatment. And the bleeding risks were similar with apixaban and aspirin.
In patients with NVAF who were ineligible for VKA therapy, clopidogrel plus aspirin reduced the risk of major vascular events, especially stroke, when compared to aspirin alone. However, the combination also increased the risk of major hemorrhage, including intracranial bleeding.
Recommendations
The authors noted that determining stroke risk in NVAF patients is difficult. So they recommend that clinicians weigh the risks and benefits of stroke prophylaxis in each patient. The authors also recommend informing patients about the potential risk of stroke and taking the patient’s preferences into account.
Clinicians should routinely offer anticoagulant therapy to patients with NVAF and a history of transient ischemic attack or stroke. On the other hand, anticoagulants might not be necessary in NVAF patients who lack additional risk factors for stroke.
Clinicians should use a risk-stratification scheme to help them identify patients at a higher risk for stroke and those with no clinically significant risk. However, anticoagulation thresholds are not necessarily definitive indicators of the need for anticoagulant therapy.
When choosing among anticoagulants, clinicians should consider the individual patient’s needs and take into account the aforementioned efficacy and safety data.
For more details, see the guidelines in Neurology.

