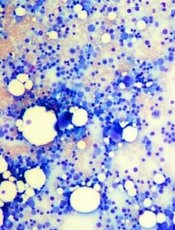
Credit: Daniel E. Sabath
Researchers say they’ve discovered a distinct bone-marrow-failure syndrome and the genetic defect that causes it.
In its natural form, the gene ERCC6L2 plays a role in DNA repair and mitochondrial function.
But investigators found evidence to suggest that mutations in ERCC6L2, and the subsequent DNA damage, were the underlying cause of tri-lineage bone marrow failure in a pair of patients with neurological dysfunction.
“New DNA sequencing technology has enabled us to identify and define a new gene defect which causes a particular type of bone marrow failure,” said Inderjeet Dokal, MD, of Queen Mary University of London in the UK.
“Clinicians treating patients with bone marrow failure should now include analysis for this gene in their investigation.”
Dr Dokal and his colleagues described this research in The American Journal of Human Genetics.
The team performed exome sequencing in 3 patients with genetically uncharacterized, tri-lineage bone marrow failure.
The patients came from consanguineous families (their parents were first-degree cousins), they had developmental delays characterized by learning disabilities, and 2 of the patients had microcephaly.
The sequencing did not uncover variations in any of the known genes associated with bone marrow failure. And the researchers could not find any obvious disease-causing variants in 1 of the patients.
However, the other 2 patients shared homozygous truncating mutations in ERCC6L2—c.1963C>T (p.Arg655*) and c.1236_1239delAACA (p.Thr413Cysfs*2). The c.1963C>T variant had already been identified, but, to the researchers’ knowledge, the other variant had not.
Additional experiments suggested that these mutations affect the subcellular localization and stability of ERCC6L2.
The investigators then speculated that ERCC6L2 plays a role in the DNA-damage response. To test that theory, they mimicked the truncating mutations by knocking down ERCC6L2 expression in human A549 cells.
This significantly reduced cell viability when the cells were exposed to the DNA-damaging agents mitomycin C and irofulven.
To further confirm their theory, the researchers looked at another marker of DNA damage. Previous research had suggested that Snf2 protein complexes are involved in the recruitment of γH2AX, a phosphorylated form of histone 2A, to sites of DNA damage.
So the team performed immunostaining with a γH2AX-specific antibody. And they found that ERCC6L2-knockdown cells displayed H2AX phosphorylation, an effect that increased upon genotoxic stress (treatment with irofulven).
These results indicate that ERCC6L2 plays a role in the DNA-damage-response pathway, and knockdown of this gene sensitizes cells to genotoxic agents.
Additional experiments showed that ERCC6L2 translocated to the mitochondria and the nucleus in response to DNA damage. And ERCC6L2 knockdown induced intracellular reactive oxygen species (ROS).
But introducing the ROS scavenger N-acetyl cysteine diminished the cytotoxicity induced by irofulven, and it halted ERCCGL2 traffic to the mitochondria and nucleus.
The investigators said these results point to a distinct bone-marrow-failure syndrome resulting from mutations in ERCC6L2.
“This is a promising finding which we hope, one day, could lead to finding an effective treatment for this type of gene defect,” Dr Dokal said. “Now [that] we know this research technique works, we plan to carry out further studies to shed more light on the genetic basis of many other cases of bone marrow failure.”

