A study of lymphoma patients receiving R-CHOP chemotherapy showed that use of the antiviral drug entecavir resulted in a lower incidence of hepatitis B virus (HBV)-related hepatitis and HBV reactivation, when compared with the drug lamivudine.
HBV reactivation is a well-documented complication of chemotherapy that can result in life-threatening liver failure, as well as delays in chemotherapy or
premature termination of treatment.
However, researchers have not identified an optimal approach to prevent HBV reactivation.
So He Huang, MD, of the Sun Yat-sen University Cancer Center in Guangzhou, China, and colleagues set out to do that. They reported their findings in JAMA alongside a related editorial.
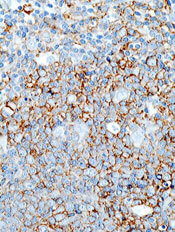
The team enrolled 121 patients with untreated diffuse large B-cell lymphoma who were receiving chemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) and were seropositive for the hepatitis B surface antigen.
Patients were randomized to receive entecavir (n=61) or lamivudine (n=60). They began taking these drugs 1 week before the initiation of R-CHOP and continued until 6 months after they completed chemotherapy.
The study was conducted from February 2008 through December 2012 at 10 medical centers in China. This trial was a substudy of a parent study designed to compare a 3-week R-CHOP regimen with a 2-week R-CHOP regimen.
Results showed that, compared to the lamivudine group, patients in the entecavir group had significantly lower rates of hepatitis (8.2% vs 23.3%, P=0.02), HBV-related hepatitis (0% vs 13.3%, P=0.003), HBV reactivation (6.6% vs 30%, P=0.001), delayed hepatitis B (0% vs 8.3%, P=0.03), and chemotherapy disruption (1.6% vs 18.3%, P=0.002).
The rate of treatment-related adverse events was not significantly different between the groups. Such events occurred in 24.6% of patients in the entecavir group and 30.0% of patients in the lamivudine group (P=0.50).
The researchers noted that entecavir is more expensive than lamivudine, so additional studies are needed to determine whether all patients who are seropositive for the hepatitis B surface antigen and are receiving rituximab-based immunosuppressive therapy should be given entecavir.
Additional studies could also help pinpoint which patients will benefit most from entecavir prophylaxis. However, if these findings are replicated, they support the use of entecavir in these patients.

