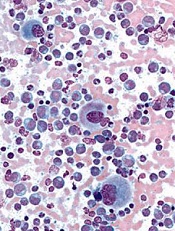
Credit: UC San Diego
Nilotinib and dasatinib, currently approved for the treatment of drug-resistant chronic myeloid leukemia (CML), provide quicker and better responses as front-line therapy than the current standard, imatinib, according to 2 international, phase 3 trials.
Complete cytogenetic responses and major molecular responses were higher among newly diagnosed CML patients treated with nilotinib or dasatinib first, compared to newly diagnosed patients treated with imatinib first.
Also, more patients treated with imatinib experienced disease progression than patients treated with second-line drugs.
In the DASISION trial, 519 treatment-naïve CML patients received 100 mg of dasatinib or 400 mg of imatinib, once daily, as front-line therapy.
In the dasatinib arm, 77% of patients had confirmed cytogenetic responses (CCyR), compared to 66% in the imatinib arm. Patients on dasatinib also reached CCyR faster than those on imatinib, 54% in 3 months vs 31% in 3 months, respectively.
Forty-six percent of patients in the dasatinib arm reached a major molecular response (MMR), compared to 28% in the imatinib group.
In the imatinib arm, 3.5% of patients experienced disease progression, compared to 1.9% in the dasatinib group.
Side effects were mostly low-grade with both drugs. However hematologic side-effects were more common in dasatinib-treated patients and low-grade side effects such as vomiting, muscle pain, and inflammation were more common in patients using imatinib.
“We’ve learned in cancer therapy that it’s important to use your big guns up front,” said Hagop Kantarjian, MD, of The University of Texas MD Anderson Cancer Center in Houston. Dr Kantarjian is the corresponding author of the DASISION study and coauthor of the ENEST study.
“We know that achieving complete cytogenetic response or major molecular response within a year of starting treatment is associated with more favorable long-term survival. Using these second-generation drugs will likely improve outcomes for patients with chronic myeloid leukemia.”
The ENEST trial of nilotinib and imatinib yielded similar results in favor of second-generation treatments.
Eight hundred thirty-six newly diagnosed CML patients were treated with 300 mg or 400 mg of nilotinib twice daily or 100 mg of imatinib once daily.
The 300 mg nilotinib arm experienced CCyR in 80% of patients, MMR in 44% of patients, and progression in less than 1% of patients. In the 400 mg nilotinib arm, 78% of patients experienced CCyR, 43% experienced MMR ,and again, less than 1% experienced disease progression.
In the same trial, only 65% of patients experienced CCyR, 22% experienced MMR, and 4% saw progression in their disease when treated with imatinib.
The median time to reach MMR was 5.7 months in the 300 mg nilotinib group, 5.8 months in the 400 mg nilotinib group, and 8.3 months in the imatinib group.
Serious side effects were uncommon for both drugs. This time, hematologic side effects were more common in patients taking imatinib, and patients taking nilotinib were more likely to experience low-grade side effects like vomiting and inflammation.
“Findings from both of these studies confirm the single-arm trials done at MD Anderson, which had shown superiority of second-generation drugs in a front-line setting,” said Dr Kantarjian.
Their findings are published online in The New England Journal of Medicine.
Currently, Jorge Cortez, MD, at MD Anderson Cancer Center, is conducting 2 single-arm clinical trials to compare the performance of the second-generation CML drugs against historical imatinib trial results.

