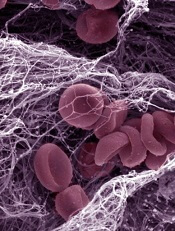
Credit: Kevin MacKenzie
The US Food and Drug Administration (FDA) has approved apixaban (Eliquis) to treat venous thromboembolism (VTE) and prevent recurrent VTE after initial therapy.
Apixaban is an oral selective factor Xa inhibitor that is already FDA approved to reduce the risk of stroke and systemic embolism in patients with nonvalvular atrial fibrillation and to prevent VTE in patients who have undergone hip or knee replacement surgery.
Apixaban’s latest FDA approval was based on results of the AMPLIFY and AMPLIFY-EXT studies.
The AMPLIFY trial
AMPLIFY included 5395 patients with confirmed, symptomatic deep vein thrombosis (DVT) or pulmonary embolism (PE) who required treatment for 6 months. They had a mean age of 56.9 years, and 89.8% of randomized patients had unprovoked VTE.
About half of patients (n=2691) were randomized to receive apixaban at 10 mg twice daily for 7 days, followed by 5 mg twice daily for 6 months.
The other half (n=2704) were randomized to the standard of care—enoxaparin at 1 mg/kg twice daily for at least 5 days until they had an INR ≥ 2 and warfarin (target INR range 2.0-3.0) for 6 months.
Apixaban proved noninferior to standard therapy in the combined primary endpoint of recurrent, symptomatic VTE (nonfatal DVT or PE) or VTE-related death. This outcome occurred in 2.3% of patients in the apixaban arm and 2.7% of patients in the standard-therapy arm (P<0.0001 for noninferiority).
Apixaban also proved superior to standard therapy with regard to bleeding. The composite endpoint of major bleeding and clinically relevant, nonmajor bleeding occurred in 4.3% of patients in the apixaban arm and 9.7% of patients in the standard-therapy arm (P<0.001).
The AMPLIFY-EXT trial
AMPLIFY-EXT included 2486 patients who had completed 6 to 12 months of anticoagulation treatment for DVT or PE. Their mean age was 56.7 years, and 91.7% of randomized patients had unprovoked VTE.
Patients were randomized to receive apixaban at 2.5 mg (n=842), apixaban at 5 mg (n=815), or placebo (n=829).
Both apixaban doses were significantly superior to placebo (P<0.001) with regard to the primary efficacy endpoint, which was recurrent VTE or all-cause death.
During the 12-month active study period, these events occurred in 3.8% of patients in the 2.5 mg arm, 4.2% of patients in the 5 mg arm, and 11.6% of patients in the placebo arm.
The primary safety endpoint was the incidence of major bleeding, and there was no significant difference among the treatment arms. Major bleeding occurred in 0.2% of patients in the 2.5 mg arm, 0.1% of patients in the 5 mg arm, and 0.5% of patients in the placebo arm.
Nevertheless, apixaban has been shown to increase the risk of bleeding and can cause serious, potentially fatal, bleeding.
Apixaban’s label includes boxed warnings detailing the increased risk of thrombotic events in patients who prematurely discontinue the drug, as well as the increased risk of epidural or spinal hematoma, which may cause long-term or permanent paralysis, in patients undergoing spinal epidural anesthesia or spinal puncture.
For more information, visit eliquis.com. The drug is under joint development by Pfizer and Bristol-Myers Squibb.

