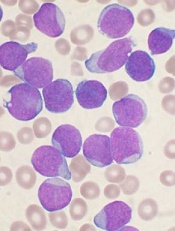
Image by Vashi Donsk
Researchers say they have characterized a subpopulation of leukemia cells that are responsible for relapse in acute lymphoblastic leukemia (ALL).
The team identified these dormant, therapy-resistant cells in mouse models of ALL and found that removing the cells from their environment makes them sensitive to treatment.
The researchers believe these findings could pave the way to better relapse prevention in patients with ALL.
“Previously, the biological principles responsible for a relapse in leukemia were not fully understood,” said study author Irmela Jeremias, MD, PhD, of Helmholtz Zentrum München in Munich, Germany.
“Our new approach is to isolate dormant cells, which gives us the first possibility of developing therapies that switch off these cells.”
Dr Jeremias and colleagues described this approach in Cancer Cell.
First, the researchers created mouse models recapitulating minimal residual disease (MRD) and relapse in ALL patients.
The team then used genetic engineering and proliferation-sensitive dyes to isolate and characterize relapse-inducing cells.
This revealed a subpopulation of leukemia cells that exhibited long-term dormancy, treatment resistance, and stemness. These cells were similar to primary ALL cells isolated from pediatric and adult patients with MRD.
However, the dormant leukemia cells found in the mice changed once they were removed from the in vivo environment. They began to proliferate and became sensitive to ex vivo treatment with chemotherapy drugs.
“[T]hese cells, once they have been dissolved out of their surroundings, are indeed susceptible to therapy and react well to therapeutics,” said study author Erbey Özdemir, a doctoral candidate at Helmholtz Zentrum München.
The researchers therefore believe that therapeutic strategies aimed at dissociating dormant leukemia cells from their protective niche might prevent relapse in ALL patients.
“This has brought us a small step closer to the global goal of preventing disease relapse in patients suffering from leukemia,” Dr Jeremias said. “It might serve as basis for new therapies that destroy resistant leukemia cells before they induce relapse.”


