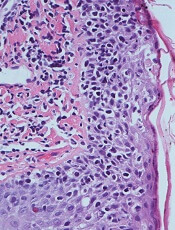
mycosis fungoides
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended that chlormethine gel (Ledaga®) be approved for use in adults with mycosis fungoides (MF).
Ledaga is a hybrid medicine of Caryolysine, which has been approved for use in the European Union since 1946.
Ledaga contains the same active substance as Caryolysine but is a gel intended for cutaneous use.
The active substance of Ledaga is chlormethine, a bifunctional alkylating agent that inhibits rapidly proliferating cells.
Hybrid drug applications rely, in part, on the results of preclinical tests and clinical trials for a reference product and, in part, on new data.
The CHMP said studies have demonstrated the satisfactory quality of Ledaga. Since Ledaga is administered as a topical agent and results in no systemic exposure, a bioequivalence study versus the reference product, Caryolysine, was not required.
The CHMP’s recommendation for Ledaga will be reviewed by the European Commission, which is expected to issue a final decision by the end of February 2017.
If approved, Ledaga will be available as a 160 μg/g gel.
Actelion Pharmaceuticals Ltd, the company developing Ledaga, has agreed to a list of recommendations from the CHMP (post-authorization measures) with regard to the release of Ledaga in Europe.
Subject to the agreed recommendations and achieving market access in different countries, a potential first launch of Ledaga could occur at the end of 2017, at the earliest.
Phase 2 study
The CHMP’s positive opinion of Ledaga is based on results of a multicenter, randomized, observer-blinded, active-controlled study of patients with stage I and IIA MF. Results from this phase 2 study were published in JAMA Dermatology.
The study enrolled 260 patients who were randomized 1:1 to receive topical treatment with Ledaga or compounded control—chlormethine HCl 0.02% compounded in Aquaphor® ointment—once daily for up to 12 months.
A response was defined as at least a 50% improvement in the baseline Composite Assessment of Index Lesion Severity score.
In the intent-to-treat population, 59% (76/130) of patients who received Ledaga achieved a clinical response, compared to 48% (62/130) of patients treated with the compounded control. The rate of complete response was 14% (n=18) and 12% (n=15), respectively.
Patients who were treated for at least 6 months were included in the efficacy-evaluable population. In this population, 77% (69/90) of patients who received Ledaga achieved a clinical response, compared to 59% (56/95) of patients treated with the compounded control. The rate of complete response was 19% (n=17) and 15% (n=14), respectively.
Reductions in mean lesion severity were seen as early as 4 weeks into the study, with further reductions observed with continuing therapy. The time to first confirmed response favored Ledaga.
The most frequent adverse reactions reported with Ledaga were skin-related—dermatitis (55%; eg, skin irritation, erythema, rash, urticaria, skin-burning sensation, pain of the skin), pruritus (20%), skin infections (12%), skin ulceration and blistering (6%), and skin hyperpigmentation (6%).
No systemic absorption of chlormethine was detected with treatment.


