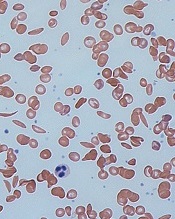
and normal red blood cells
Image by Graham Beards
Researchers say they have identified a genetic risk profile that can be used to predict which patients with sickle cell anemia (SCA) are likely to develop chronic kidney disease (CKD).
The team found evidence to suggest that a profile incorporating APOL1 G1/G2, α-thalassemia, and BCL11A can help physicians categorize SCA patients as having a high or low risk of CKD.
The researchers reported these findings in Haematologica.
Identifying SCA patients at the greatest risk of CKD can help physicians develop proactive, individualized strategies to reduce the high rate of early mortality due to CKD, said study author Santosh Saraf, MD, of the University of Illinois at Chicago.
“We looked at the genetic factors already known to be associated with kidney disease or the degree of red blood cell hemolysis and examined the relationship they had with the condition in sickle cell patients,” Dr Saraf said.
“Our hypothesis was that a genetic risk profile that integrated APOL1, α-thalassemia, and BCL11A would improve our ability to predict a patient’s risk for developing chronic kidney disease.”
To test this theory, Dr Saraf and his colleagues recruited 262 adult patients with SCA treated at a single center between 2010 and 2016. The team collected patient data, drew blood, analyzed genetic markers, and prospectively followed the patients to see if they developed CKD.
Stratification
The researchers used their genetic profile to stratify patients according to risk for CKD.
Patients were considered high-risk if they had APOL1 G1/G2 and wild-type BCL11A but did not have α-thalassemia.
Patients were considered low-risk if they were negative for APOL1 G1/G2 but had α-thalassemia (either α-/αα or α-/α-) and the BCL11A rs1427407 T allele (either G/T or T/T).
The researchers defined all other combinations as intermediate-risk.
The team found the genetic profile identified SCA patients at high and low risk for albuminuria or an estimated glomerular filtration rate less than 60 mL/min/1.73m2.
The researchers also said application of the genetic profile revealed progressively higher rates of CKD progression.
Mechanisms
Dr Saraf and his colleagues noted that homozygosity or compound heterozygosity for APOL1 G1/G2 is the strongest genetic association for CKD in African Americans, and APOL1 G1/G2 is associated with proteinuria and albuminuria in SCA patients.
The researchers pointed out that APOL1 G1/G2 variants associate with CKD in African
Americans by unknown mechanisms, but the team found an association with
hemolysis in SCA, as reflected by hemoglobinuria.
As for α-thalassemia, it’s associated with reduced hemolysis and protection from albuminuria. The researchers said α-thalassemia reduces hemolysis in SCA by decreasing the
intra-erythrocyte concentration of sickle hemoglobin (HbS) and reducing
HbS polymerization.
Finally, Dr Saraf and his colleagues noted that BCL11A rs1427407 leads to higher fetal hemoglobin (HbF) levels, reduced hemolysis, and amelioration of SCA-related complications. The team said the BCL11A rs1427407 T variant leads to decreased function of BCL11A at the HbF promoter and therefore increases HbF, leading to decreased HbS polymerization.
“The results of this study are encouraging,” Dr Saraf said. “By understanding more about the genetic risk factors of kidney disease in sickle cell patients, we are one step closer to improving the length and quality of life for the millions of people worldwide living with sickle cell disease.”
“Using combinations of genes to better predict complications in sickle cell anemia is a new approach,” added study author Victor Gordeuk, MD, of the University of Illinois at Chicago.
“The results of this study indicate that it is effective and probably can be improved on in the future to be an important part of our evaluation of patients.”
The researchers said the small sample size and observational nature of this study are limitations, and they hope to validate the results with larger studies.


