The National Comprehensive Cancer Network (NCCN) has published new clinical practice guidelines for myeloproliferative neoplasms (MPNs).
The current guidelines focus on the management of patients with myelofibrosis (MF), but NCCN said recommendations for managing essential thrombocythemia (ET) and polycythemia vera (PV) will be included in subsequent versions of the NCCN guidelines for MPNs.
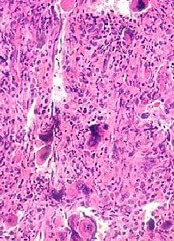
The new guidelines provide recommendations on the workup and diagnosis of primary MF, post-ET MF, and post-PV MF.
The document also includes recommendations for managing MF-associated anemia, supportive care options, and treatment recommendations according to a patient’s risk group.
Treatment of low-risk MF
The guidelines recommend that patients with low-risk, asymptomatic MF be observed or enrolled in a clinical trial. They should be monitored for progression every 3 to 6 months.
Patients with low-risk, symptomatic MF should receive ruxolitinib or interferons or be enrolled on a clinical trial. They should be monitored for progression every 3 to 6 months.
If patients respond to treatment, they should continue to receive it. If they do not respond or lose their response, they should receive ruxolitinib or interferons or be enrolled on a clinical trial. If these patients progress, they should be treated according to their risk category.
Intermediate-1-risk MF
Patients with intermediate-1-risk MF should be assessed for symptom burden and observed if asymptomatic. If symptomatic, they should receive ruxolitinib, be enrolled on a clinical trial, or undergo allogeneic hematopoietic stem cell transplant (HSCT).
Patients should be monitored for response and progression every 3 to 6 months. If they respond to treatment, they should continue to receive it.
If patients do not respond or lose their response, they should be observed, receive ruxolitinib, be enrolled on a clinical trial, or undergo allogeneic HSCT. If these patients progress, they should be treated according to their risk category.
Intermediate-2- or high-risk MF
Patients who are transplant candidates should receive allogeneic HSCT.
Patients who are ineligible for transplant should be assessed for symptom burden. Those with a platelet count of 50,000 or lower should be considered for a clinical trial.
Those with higher platelet counts should receive ruxolitinib or be enrolled on a clinical trial. They should be monitored for response or progression every 3 to 6 months.
If these patients respond to treatment, they should continue on that treatment. If they do not respond or lose their response, the patients should be monitored for progression.
If they progress and are candidates for transplant, these patients should receive hypomethylating agents or chemotherapy to induce remission, followed by HSCT.
If the patients progress and are ineligible for transplant, they should be enrolled on a clinical trial or receive hypomethylating agents or chemotherapy.
For patients who are ineligible for transplant and only have symptomatic anemia, they should receive treatment to manage that anemia. The guidelines list a range of treatment options.
“The management of MPNs has been variable in the past and largely driven by review articles and individual opinions,” said Ruben A. Mesa, MD, chair of the NCCN Guidelines Panel for MPN.
“The NCCN Guidelines Panel for MPN hopes these inaugural guidelines will help leverage the evidence base in MPN care for clear, well-informed treatment guidelines to hopefully improve quality of care and provide better outcomes for patients with MPN.”
Dr Mesa is scheduled to present the new NCCN guidelines during the NCCN 11th Annual Congress: Hematologic Malignancies™ on September 30, in a session titled, “Myeloprofilerative Neoplasms and Myelofibrosis: Evolving Management.”


