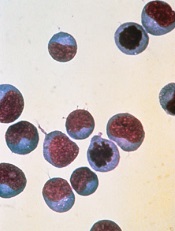
Credit: NIAID
The US Food and Drug Administration (FDA) has granted accelerated approval for blinatumomab (Blincyto) to treat adults with relapsed or refractory Philadelphia chromosome-negative precursor B-cell acute lymphoblastic leukemia (ALL).
Blinatumomab is a bispecific T-cell engager (BiTE®) antibody construct designed to direct the body’s T cells against target cells expressing CD19, a protein found on the surface of B cells.
Blinatumomab is the first anti-CD19 drug to receive FDA approval. It will be available as a 35 mcg single-use vial.
“Immunotherapies, especially Blincyto with its unique mechanism of action, are particularly promising for patients with leukemia,” said Richard Pazdur, MD, director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
“Recognizing the potential of this novel therapy, the FDA worked proactively with the sponsor under our breakthrough therapy designation program to facilitate the approval of this novel agent.”
Approval details
The FDA granted blinatumomab accelerated approval based on clinical data showing the drug has an effect on a surrogate endpoint reasonably likely to predict clinical benefit to patients.
Before granting the drug full approval, the FDA is requiring that blinatumomab’s manufacturer, Amgen, conduct a study to verify that the drug improves survival in patients with relapsed or refractory Philadelphia-negative precursor B-cell ALL.
Blinatumomab was approved with a boxed warning detailing the risk of cytokine release syndrome and neurological toxicities. The FDA also approved the drug with a Risk Evaluation and Mitigation Strategy, which consists of a communication plan to inform healthcare providers about the serious risks and the potential for preparation and administration errors.
Blinatumomab was approved more than 5 months ahead of the date the FDA was scheduled to complete review of the drug’s application (May 19, 2015).
The agency had granted blinatumomab breakthrough therapy designation, priority review, and orphan product designation because Amgen demonstrated through preliminary clinical evidence that the drug may offer a substantial improvement over available therapies.
That evidence came in the form of a phase 2 study, the results of which were presented at the 19th Congress of the European Hematology Association (EHA) in June.
Trial results
Researchers evaluated blinatumomab monotherapy in 189 patients with relapsed or refractory B-cell ALL and a median age of 39 (range, 18-79). The patients received blinatumomab by continuous intravenous infusion—4 weeks on and 2 weeks off—for up to 5 cycles.
Thirty-three percent of patients achieved a complete remission, and 9% achieved a complete remission with partial hematologic recovery. Seventy-one percent of these patients were negative for minimal residual disease.
The median relapse-free survival was 5.9 months.
Major toxicities were related to cytokine release syndrome, but cytopenias and central nervous system events were also common. The most frequent adverse events were pyrexia (59%), headache (35%), and febrile neutropenia (29%).
The most frequent grade 3 or higher adverse events were febrile neutropenia (26%), anemia (15%), and neutropenia (15%). Two percent of patients had grade 3 or higher cytokine release syndrome.
The most common grade 3 or higher nervous system events were headache (4%), encephalopathy (3%), and ataxia (2%). Three patients (2%) had grade 5 events considered treatment-related—2 with sepsis and 1 with Candida infection.


