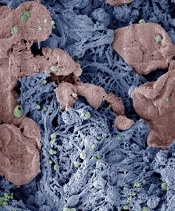
form clots in injured liver
Image courtesy of Erin Lavik
PHILADELPHIA—Researchers say they have developed nanoparticles that can congregate at sites of injury and speed blood clotting in vitro and in vivo.
The nanoparticles are designed to bind with activated platelets and help them join together to form clots faster.
The nanoparticles have helped stop bleeding and improved animals’ survival in different models of injury, without producing off-target clotting.
“When you have uncontrolled internal bleeding, that’s when these particles could really make a difference,” said Erin B. Lavik, ScD, of the University of Maryland, Baltimore County (UMBC) in Baltimore, Maryland.
“Compared to injuries that aren’t treated with the nanoparticles, we can cut bleeding time in half and reduce total blood loss.”
Dr Lavik discussed this work at the 252nd National Meeting & Exposition of the American Chemical Society.
She and her colleagues have been testing different versions of these nanoparticles for years. They previously reported results with the particles in 2012 and 2014.
The current nanoparticles are made from polylactic acid or polylactic co-glycolic acid. Dr Lavik said that by using the 2 different materials, the researchers can change the temperature at which the nanoparticles melt. Thus far, the team has developed nanoparticles that are stable up to 50° C (122° F).
The nanoparticles have an outer coating of polyethylene glycol and an attached peptide—RGD—that enables them to bind to natural platelets. Dr Lavik said the researchers chose RGD because platelets have receptors for that peptide, it’s ubiquitous in the body, and it wouldn’t alter the chemistry of the nanoparticles.
The researchers have tested the nanoparticles in a femoral injury model, a liver injury model, and blast injury model. The team has also started testing in models of brain and spinal cord injury, but the results are “very preliminary,” according to Dr Lavik.
In the femoral injury model, the nanoparticles halved bleeding time when compared to no treatment. In both the liver injury model and the blast injury model, the nanoparticles stopped bleeding and improved survival.
Dr Lavik said these experiments have shown that the nanoparticles successfully speed clotting, and the clots formed are mechanically robust.
The nanoparticles also clear the body easily. When the particles are bound into a clot, they stay as long as the clot remains. They begin to degrade once the clot does and clear out of the bloodstream quickly.
Dr Lavik said the researchers haven’t seen non-specific clotting with the nanoparticles yet. However, this side effect remains a possibility because the particles are designed to bind to activated platelets, which may not be confined to the site of injury.
One unfortunate side effect occurred with an earlier version of the nanoparticles. They triggered an immune response, activating complement in pig’s blood. However, the researchers were able to modify the particles to reduce complement activation and the accompanying complications.
In future studies, Dr Lavik and her colleagues plan to test whether the new nanoparticles activate complement in human blood. The team also aims to verify that the nanoparticles don’t cause non-specific clotting.


