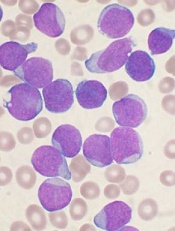
Image by Vashi Donsk
Screening for genetic abnormalities can provide a more accurate prediction of outcomes in children with relapsed B-cell precursor acute lymphoblastic leukemia (BCP-ALL), according to a study published in Blood.
Researchers found that mutations or deletions in TP53, NR3C1, BTG1, and NRAS were associated with inferior outcomes in relapsed BCP-ALL.
And screening for these abnormalities could improve upon the predictive accuracy of clinical risk factors.
“Current methods used to guide treatment for relapsed leukemia are not accurate enough, with some children believed to have a good chance of survival actually responding very poorly to chemotherapy,” said study author Anthony Moorman, PhD, of Newcastle University in Newcastle upon Tyne, UK.
“Screening patients at relapse for key genetic abnormalities that influence outcome will ensure that treatment can be personalized, thereby improving their chances of survival.”
For this study, Dr Moorman and his colleagues analyzed cytogenetic data from 427 children with relapsed BCP-ALL and screened 238 patients with a marrow relapse for certain copy number alterations and mutations.
According to univariate analysis, alterations in TP53, NR3C1 deletions, and BTG1 deletions were significantly associated with patient outcomes.
Patients with TP53 alterations had a higher risk of progression (hazard ratio [HR]=2.36, P<0.001) and death (HR=2.56, P<0.001), as did patients with deletions in NR3C1 and BTG1.
Because both NR3C1 and BTG1 are implicated in resistance to glucocorticoids and the deletions are mutually exclusive, the researchers considered the effect of the deletions together. So for patients with NR3C1 and BTG1 deletions, the HR for progression was 2.15 (P=0.002), and the HR for death was 1.91 (P=0.015).
Patients with NRAS mutations had an increased risk of progression and death as well, but this did not reach statistical significance.
The researchers also found that patients who were standard risk according to clinical characteristics but, at the time of relapse, had one or more high-risk genetic abnormalities had poorer outcomes.
Standard-risk patients with a TP53 alteration had an increased risk of death (HR=2.56, P<0.001), as did standard-risk patients with NR3C1 and BTG1 deletions (HR=1.91, P=0.015).
Standard-risk patients with NRAS mutations and high hyperdiploidy had an increased risk of progression (HR=3.17, P=0.026) and death (HR=3.41, P=0.032).
The researchers concluded that the outcomes of clinical standard-risk patients with high-risk cytogenetics were equivalent to outcomes of clinical high-risk patients.
The team therefore believes that screening BCP-ALL patients for the aforementioned genetic abnormalities at relapse will improve patient stratification and outcomes.


