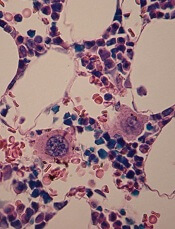
in the bone marrow
A low-intensity type of laser therapy could provide a non-invasive, drug-free treatment option for thrombocytopenia, according to research published in Science Translational Medicine.
Researchers found that low-level laser (LLL) therapy increased the generation of platelets from megakaryocytes in vitro and had the same effect in mouse models of thrombocytopenia.
The team also identified the probable mechanism underlying this effect.
“Our study reveals, for the first time, that low-level laser therapy enhances platelet production in animals with thrombocytopenia but not in normal controls,” said study author Mei X. Wu, PhD, of Massachusetts General Hospital in Boston.
“This result suggests that a safe, drug-free method that does not depend on donated blood products can be developed for treating or preventing thrombocytopenia.”
LLLs emit low-powered laser light that does not heat its target tissue. LLLs are known to protect the function of mitochondria, and several conditions associated with impaired platelet production are characterized by abnormalities in the mitochondria of cells that give rise to platelets.
Dr Wu and her colleagues conducted a number of experiments to investigate whether LLLs’ ability to protect mitochondrial function could mitigate several forms of thrombocytopenia.
The team found that LLL treatment of megakaryocytes increased their size, accelerated the formation of proplatelets, and doubled the production of platelets.
Infusion of LLL-treated megakaryocytes into mice led to greater platelet production than did infusion of megakaryocytes treated with normal light.
One of the keys to determining the number of platelets generated from megakaryocytes was mitochondrial production of the energy molecule ATP.
LLL treatment greatly increased mitochondrial generation in polyploid megakaryocytes, but the increase was only slight in less mature megakaryocytes with only 2 copies of each chromosome.
Whole-body LLL treatment of mice with radiation-induced thrombocytopenia spurred the rapid maturation of megakaryocytes and restored platelet levels in a light-dose-dependent fashion.
Platelets from LLL-treated mice had normal structure and function. LLL treatment of normal mice did not raise levels of either megakaryocytes or platelets.
LLL treatment also restored platelet levels in mice with the autoimmune form of thrombocytopenia or with thrombocytopenia caused by chemotherapy.
In cultured human megakaryocytes, LLL treatment at dosage levels similar to those used in mice increased ATP production and platelet generation.
Dr Wu noted that LLL’s lack of an effect in animals without thrombocytopenia indicates it would probably avoid the potential complications of current drug treatments for thrombocytopenia, which act by increasing the production of megakaryocytes from their progenitors in the bone marrow.
“Directly stimulating the differentiation of [megakaryocytes] the way all current drugs do risks clotting if platelet levels rise too high,” Dr Wu said. “LLL appears to enhance [megakaryocytes’] inherent ability to produce platelets most effectively in response to low platelet levels in the circulation, a response that stops when platelet levels are normalized.”
“The fact that treatment only has an effect in polyploid cells, which are very rare, implies that it would not increase production of mitochondria in cancer cells or other cells. In fact, while LLL has been employed in research and in clinical treatment for decades, this is the first study reporting that it can promote mitochondrial biogenesis.”
Dr Wu added that the current primary obstacle to testing LLL in humans is the lack of a device large enough to treat either the entire body or enough bones to stimulate sufficient platelet production by megakaryocytes within the bone marrow, something her team plans to address.
She also noted that, while LLL will probably be beneficial for treatment of many forms of acquired thrombocytopenia, it may not be effective when the condition is caused by inborn genetic defects.


