Preclinical research suggests that some leukemia cells harvest energy resources from normal cells during chemotherapy, and this helps the leukemia cells survive and thrive after treatment.
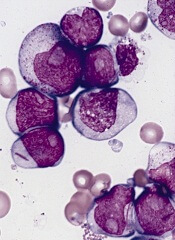
Investigators found that acute myeloid leukemia (AML) cells are capable of stealing mitochondria from stromal cells, and these stolen mitochondria give an energy boost to surviving AML cells, which helps fuel the leukemia’s resurgence after chemotherapy.
“There are multiple mechanisms for resistance to chemotherapy, and it will be important to target them all in order to eliminate all leukemic cells,” said Jean-François Peyron, PhD, of the Centre Méditerranéen de Médecine Moléculaire (C3M) in Nice, France.
“Targeting this protective mitochondrial transfer could represent a new strategy to improve the efficacy of the current treatments for acute myeloid leukemia.”
Dr Peyron and his colleagues described their discovery of the mitochondrial transfer in Blood.
The team conducted their experiments using cell cultures and mouse models of AML. They found that nearly all AML cells died when exposed to chemotherapy drugs, but some survived. And these cells issued a “mayday” signal that “tricked” nearby non-cancerous cells into yielding their mitochondria to the AML cells, thus strengthening the leukemia cells.
“Mitochondria produce the energy that is vital for cell functions,” explained study author Emmanuel Griessinger, PhD, also of C3M.
“Through the uptake of mitochondria, chemotherapy-injured acute myeloid leukemia cells recover new energy to survive.”
The AML cells were found to increase their mitochondria mass by an average of 14%. This increase led to a 1.5-fold increase in energy production and significantly better survival rates. That is, the leukemia cells that had a high level of mitochondria were also more resistant to the chemotherapy.
The investigators observed the phenomenon in several types of leukemia cells, most notably leukemia-initiating cells. The team said this finding may explain why it can be difficult to treat AML and other cancers.
They also believe these findings offer new hope for developing better treatments for AML. If researchers can find a way to interfere with the transfer of mitochondria, that could reduce the risk of relapse.
The study may also shed light on other cancer types. Similar mechanisms may be at play in other hematologic malignancies and even solid tumors, according to the investigators.
For now, the team’s next step for this research is to identify the mechanism underlying the transfer of mitochondria in AML.


