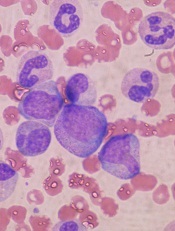
in the bone marrow
Scientists say that, using a model of the hematopoietic system, they have determined which signaling pathways play an essential role in the self-renewal of hematopoietic stem cells (HSCs).
They found that a particularly important role in this process is the interactive communication with surrounding tissue cells in the bone marrow.
Robert Oostendorp, PhD, of Klinikum Rechts der Isar der Technischen Universität München in Munich, Germany, and his colleagues described these findings in Stem Cell Reports.
The team noted that, in steady-state conditions, HSCs are maintained as slow-dividing clones of quiescent cells. However, when stress occurs, such as an accident that leads to substantial blood loss or the defense against a pathogen requires more blood cells in the course of an infection, HSCs are activated.
In response, the entire hematopoietic system switches from “standby” mode into a state of alert. The activated HSCs generate new blood cells to counteract the blood loss or combat the pathogen. At the same time, self-renewal keeps the stem cell pool replenished.
This switch is accompanied by a complex communication process between the HSCs and tissue cells—an area that had not previously been examined in depth.
“In our study, we set out to establish which tissue signals are important to stem cell maintenance and functionality, and which HSC signals influence the microenvironment,” Dr Oostendorp said.
He and his colleagues used mixed cultures of tissue cells and HSCs to investigate how these cell types interact.
The scientists analyzed factors that are upregulated or downregulated in the interplay between tissue cells and HSCs. And they linked these findings with the signaling pathways described in existing literature.
The team then consolidated this information in a bioinformatics computer model. And they conducted extensive cell experiments to confirm the computer-generated signaling pathway model.
“The outcome was very interesting indeed,” Dr Oostendorp said. “The entire system operates in a feedback loop. In ‘alert’ mode, the stem cells first influence the behavior of the tissue cells, which, in turn, impact on the stem cells, triggering the self-renewal step.”
In alert mode, HSCs emit signaling substances, which induce tissue cells to release the connective tissue growth factor (CTGF) messenger. This is essential to maintain the HSCs through self-renewal. In the absence of CTGF, HSCs age and cannot replenish the stem cell pool.
“Our findings could prove significant in treating leukemia,” Dr Oostendorp noted. “In this condition, the stem cells are hyperactive, and their division is unchecked. Leukemic blood cells are in a constant state of alert, so we would expect a similar interplay with the tissue cells.”
To date, however, the focus here has been limited to stem cells as the actual source of the defect.
“Given what we know now about feedback loops, it would be important to integrate the surrounding cells in therapeutic approaches too, since they exert a strong influence on stem cell division,” Dr Oostendorp concluded.


