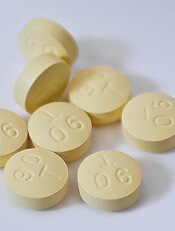
Photo courtesy of AstraZeneca
The US Food and Drug Administration (FDA) has announced that confusion between the anticoagulant Brilinta (ticagrelor) and the antidepressant Brintellix (vortioxetine) is resulting in the wrong medication being prescribed or dispensed.
The FDA found the main reason for the confusion is the similarity of the drugs’ brand names.
None of the reports the FDA received indicate that a patient ingested the wrong medication. However, the FDA continues to receive reports of prescribing and dispensing errors.
As of June 2015, the agency has received 50 reports of name confusion between Brintellix and Brilinta. The FDA confirmed that the wrong medication was dispensed to a patient in 12 of the cases and may have been dispensed in 3 additional cases.
About the medications
Brilinta is a P2Y12 platelet inhibitor approved for use in patients with acute coronary syndrome to reduce the rate of thrombotic cardiovascular events. The drug comes in the form of a round, yellow tablet with a “90” above a “T” stamped on one side.
Brintellix is a selective serotonin reuptake inhibitor used to treat major depressive disorder in adults. The medication comes in the form of a tear-shaped tablet stamped with “TL” on one side of the tablet and a number that indicates the tablet strength on the other side. It varies in color depending upon the strength prescribed.
About the error reports
As of June 2015, the FDA has received 50 medication error reports describing brand name confusion with Brintellix (vortioxetine) and Brilinta (ticagrelor). In most cases, Brintellix was mistaken as Brilinta.
Some of the contributing factors to the name confusion included the following:
- Both brand names begin with the same 3 letters
- Both brand names are presented when selecting medications in a computerized physician order entry (CPOE) system
- The pharmacist was not familiar with the new medication Brintellix and so dispensed Brilinta
- The brand names look and sound similar.
Of these 50 reports, the wrong medication was actually dispensed in 12 cases and was possibly dispensed in 3 additional cases but could not be confirmed based on the case narrative information. None of the reports indicated a patient had ingested the wrong medication.
However, in one case, Brintellix was misinterpreted as Brilinta, and the pharmacist did not dispense any medication because the patient had a contraindication to antiplatelet therapy. As a result, the patient went untreated for the psychiatric indication for an unreported period.
In the 12 cases where a wrong medication was actually dispensed, the reports showed that, in 6 cases, the error occurred when prescribing the medication.
Five of these prescribing errors occurred during CPOE. Some CPOE systems auto-populate or present a drop-down menu after the first 3 letters are typed, at which point a prescriber can select the wrong medication.
In the other 6 cases, the error occurred during dispensing of the medication.
FDA recommendations
The FDA is recommending that healthcare professionals reduce the risk of name confusion when prescribing these medications by including the generic names, indications for use, correct dosage, and directions for use.
Healthcare professionals should also ensure that patients understand what their medication is used to treat and encourage patients and their caregivers to read the Medication Guides provided with their Brintellix and Brilinta prescriptions.
Healthcare professionals and patients can report name confusion and medication errors involving Brintellix and Brilinta to the FDA MedWatch Program.


