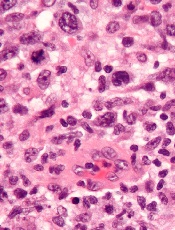
anaplastic large cell lymphoma
The histone deacetylase inhibitor belinostat can produce durable responses in patients with relapsed/refractory peripheral T-cell lymphoma (PTCL), results of the BELIEF study suggest.
The overall response rate (ORR) was low in this heavily pretreated population, at about 26%.
But responses occurred across PTCL subtypes and irrespective of a patient’s prior treatment, and the median duration of response was 13.6 months.
The researchers said toxicity was manageable, and the rate of grade 3/4 thrombocytopenia was low.
“This is a very exciting time in the treatment of patients with PTCL,” said Owen O’Connor, MD, PhD, of Columbia University Medical Center in New York, New York.
“At long last, we finally have tools in the therapeutic armamentarium to help our patients. Belinostat represents the latest drug approved for patients with [relapsed/refractory] PTCL that has relatively few side effects and produces long durations of benefit, even in patients who have received multiple conventional treatments in the past.”
Dr O’Connor and his colleagues reported results with belinostat in the Journal of Clinical Oncology. The research was sponsored by Spectrum Pharmaceuticals, Inc., the company developing belinostat (as Beleodaq).
BELIEF was a single-arm, phase 2 trial that enrolled 129 patients with relapsed/refractory PTCL. One hundred and twenty patients were evaluable. They had a median age of 64 (range, 29-81), and roughly half of patients were female.
PTCL subtypes included PTCL-not otherwise specified (n=77), angioimmunoblastic T-cell lymphoma (n=22), ALK-negative anaplastic large cell lymphoma (n=13), ALK-positive anaplastic large cell lymphoma (n=2), enteropathy-associated T-cell lymphoma (n=2), nasal type extranodal natural killer T-cell lymphoma (n=2), and hepatosplenic T-cell lymphoma (n=2).
The patients had received a median of 2 prior therapies (range, 1-8), including multi-agent and single-agent regimens, as well as transplant.
For this study, the patients received belinostat (1000 mg/m2) as daily, 30-minute infusions on days 1-5 every 21 days until disease progression or unacceptable toxicity.
Response and survival
The study’s primary endpoint was ORR, as assessed by an independent review committee using the International Working Group criteria. The ORR was 25.8% (n=31), including 13 complete responses (10.8%) and 18 partial responses (15%).
The median time to response was 5.6 weeks, and the median duration of response was 13.6 months by International Working Group criteria. The median duration of response based on the date of first response to progressive disease or death was 8.4 months.
Among patients who achieved a complete response, the median duration of response was not reached and exceeded 29 months. The longest ongoing patient response is more than 36 months.
The median progression-free survival was 1.6 months, and the median overall survival was 7.9 months.
Forty-six patients were censored for overall survival because they were alive at the data cutoff point. Seven of these patients continued to receive belinostat. Five were in complete response, 1 had a partial response, and 1 had stable disease.
Twelve patients underwent stem cell transplant after belinostat, and 10 of these patients were still alive at the data cutoff. Their overall survival ranged from 9.4 months to 22.9 months.
Adverse events
Treatment-emergent adverse events (AEs) occurred in 96.9% of patients, and treatment-related AEs occurred in 83.7%. The most common treatment-related AEs were nausea (38.0%), fatigue (28.7%), and vomiting (24.0%). Serious AEs occurred in 47.3% of patients.
Grade 3/4 related AEs were reported in 61.2% of patients, and the most common were anemia (10.9%), thrombocytopenia (7.0%), dyspnea (6.2%), neutropenia (6.2%), fatigue (5.4%), and pneumonia (5.4%).
About 12% of patients underwent a dose reduction due to AEs, 19.4% discontinued treatment due to AEs, and 10.9% of these AEs were considered treatment-related.
Twenty-two patients (17.1%) died, 12 (9.3%) of progressive disease and 10 (7.8%) of AEs. One death was considered related to belinostat. This patient had tolerated 9 cycles of the drug without complications but had elevated liver function tests at the start of cycle 10 that subsequently led to death from toxic liver failure.


