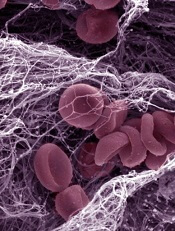
Image by Kevin MacKenzie
AMSTERDAM—The oral anticoagulant edoxaban compares favorably with warfarin as treatment for recurrent venous thromboembolism (VTE), according to results of the Hokusai-VTE trial.
Edoxaban given after initial low molecular weight heparin (LMWH) proved equally as effective as warfarin given after LMWH.
And patients treated with edoxaban were less likely to experience clinically relevant bleeding than patients who received warfarin.
Results of the trial also offer new insight into a previously under-represented subgroup of patients with pulmonary embolism (PE), suggesting that treatment for this group might need to be different than for other VTE patients, said lead investigator Harry R. Büller, MD, of the Academic Medical Center in Amsterdam.
Dr Büller presented these findings at the 2013 European Society of Cardiology Congress, which is taking place August 31 through September 4. The study was also published in NEJM on September 1.
“What makes this study unique is new insight that there are subgroups in which we might need to revisit what we currently think about the treatment of VTE,” Dr Büller said.
The Hokusai-VTE trial included a broad spectrum of VTE patients, including a large subgroup (30%) of patients with PE and right ventricular dysfunction, and another subgroup (20%) at high risk for bleeding due to renal impairment and low body weight.
In total, 4921 patients with deep vein thrombosis and 3319 with PE received initial subcutaneous LMWH therapy and were then randomized to receive edoxaban or warfarin daily for 3 to 12 months.
Patients at a higher risk for bleeding—ie, those with creatinine clearance of 30 to 50 mL/min or body weight below 60 kg—received 30 mg of edoxaban. The rest of the patients in the edoxaban arm received 60 mg. Warfarin patients were dosed according to standard of care.
Overall, edoxaban proved as effective as warfarin. Recurrent symptomatic VTE occurred in 3.2% and 3.5% of patients, respectively (P<0.001 for noninferiority).
However, in the subgroup of patients with PE and evidence of right ventricular dysfunction, efficacy was superior with edoxaban—3.3% and 6.2%, respectively.
Edoxaban proved superior when it came to the primary safety outcome as well. Clinically relevant bleeding occurred in 8.5% of edoxaban-treated patients and 10.3% of warfarin-treated patients (P=0.004 for superiority).
In the edoxaban arm, there were 2 fatal bleeds and 13 non-fatal bleeds in a critical site. With warfarin, there were 10 fatal bleeds and 25 non-fatal bleeds in a critical site.
“By halving the daily dose of edoxaban to 30 mg [among patients at high risk of bleeding], efficacy was maintained, with significantly less bleeding than observed in the warfarin group,” Dr Büller said.
In this high-risk subgroup, clinically relevant bleeding occurred in 7.9% of those treated with edoxaban, compared to 12.8% of those treated with warfarin. And recurrent symptomatic VTE occurred in 3.0% and 4.2%, respectively.
Previous trials of oral anticoagulants have not identified these specific subgroups, Dr Büller said.
“Our findings are likely to be generalizable in a global setting,” he added. “We included patients with both provoked and unprovoked venous thromboembolism, and treatment durations varied from 3 to 12 months at the discretion of the treating physician.”
This study was supported by Daiichi Sankyo, the company developing edoxaban.


