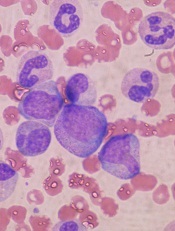
in the bone marrow
Scientists say they have identified a family of multipotent progenitor (MPP) cells that are the first to arise from hematopoietic stem cells (HSCs).
The team said their discovery, published in Cell Stem Cell, raises the possibility that, by manipulating the fates of MPPs or HSCs, researchers could one day help overcome imbalances and deficiencies that can arise in the blood system due to aging or leukemia.
Similar imbalances can render patients vulnerable immediately following HSC transplants, especially following umbilical cord transplants, said study author Emmanuelle Passegué, PhD, of the University of California San Francisco.
Via experiments in mice, Dr Passegué and her colleagues found that HSCs “make educated decisions” when it comes time to differentiate.
“Previously, researchers thought that the developmental paths of daughter cells were randomly specified by the HSC, but we conclude that the HSC normally responds appropriately to signals in the environment, making the different MPPs in parallel, but at different speeds and in different amounts to meet the body’s needs,” Dr Passegué said.
To uncover these findings, she and her colleagues investigated patterns of gene expression and cell signaling that determine which developmental paths are favored when relatively rare HSCs spin off daughter cells. The team also explored HSCs’ responses during transplant.
The researchers found that the first daughter cells that arise from HSCs are already distinct, favoring the development of different specialized cell lineages.
The team identified two types of daughter cells, MPP2 and MPP3, which, under normal conditions, are rare. These cells work together with more common daughter cells, MPP4 cells, to control blood production.
MPP2 cells favor the production of platelets and red blood cells, while MPP3 cells favor production of inflammatory cells.
MPP4 cells are the main producers of lymphocytes that fight specific disease pathogens, but the researchers showed that MPP4 cells can easily be re-educated to make many inflammatory cells when regenerative needs are high, as they are following a transplant.
The team found that, during transplant, regenerating HSCs limit their own self-renewal and instead go to work overproducing MPP2 and MPP3 cells that quickly produce needed red blood cells, platelets, and inflammatory cells. Only later does MPP4 production return to normal, enabling the immune system to replenish lymphocytes.
“It will be compelling to test whether the developmental pathways leading to cell specialization can be manipulated to favor production of specific lineage-biased MPPs in order to optimize blood recovery following hematopoietic injury or to rebalance the output of various cell lineages in an aging or deregulated blood system,” Dr Passegué said.


