Image from PLOS ONE
A T-cell therapy designed to mitigate graft-vs-host disease (GVHD) is both feasible and safe, according to results of a pilot study published in Molecular Therapy.
To create this therapy, researchers transduced donor T cells with γ-retroviruses carrying a CD34-TK75 fusion gene.
The team said this allows them to track the cells via PET/CT and induce apoptosis by administering the antiviral drug ganciclovir if patients begin showing signs of GVHD.
“If donor T cells expand and cause severe graft-vs-host disease, we can give the patient ganciclovir, and it should kill the T cells and stop the process,” said study author John F. DiPersio, MD, PhD, of the Washington University School of Medicine in St Louis, Missouri.
Dr DiPersio and his colleagues tested the CD34-TK75-enriched T cells in 8 patients—4 with acute myeloid leukemia and 4 with myelodysplastic syndromes—who relapsed after allogeneic transplant. Six patients underwent [18F]FHBG PET/CT to track the T cells at several time points after infusion.
Patients received T-cell infusions ranging from 0.1 × 106 cells/kg to 1.3 × 106 cells/kg. Seven of the 8 patients received chemotherapy before T-cell infusion.
Four patients achieved a complete remission, 1 had progressive disease, and 3 patients died before the researchers could evaluate them for response.
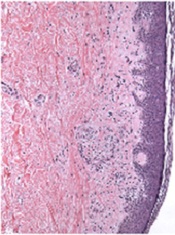
Two patients developed GVHD—1 before T-cell infusion and 1 after. The patient who developed GVHD before infusion had grade 2 liver GVHD that resolved after an increased dose of steroids. The patient ultimately died of relapsed leukemia.
The patient who developed GVHD after T-cell infusion did not respond to chemotherapy or T-cell infusion. At 64 days after infusion, he exhibited symptoms consistent with grade 4 liver GVHD. He was treated with high-dose steroids and ganciclovir but did not respond. His primary cause of death was relapsed/progressive disease.
The mean overall survival after T-cell infusion was 165 days, 4 patients were still alive at 6 months, and 1 patient lived 408 days. All of the patients ultimately died.
The researchers said they did not detect any replication competent retrovirus or any antibodies against CD34-TK in any of the patients. The team also said there were no toxicities related to the CD34-TK75-enriched T cells.
Among patients who underwent imaging, there was no clear distinction between the [18F]FHBG biodistribution at baseline and later time points. And there was no difference between images in the patient who developed GVHD after infusion and patients who did not.
Past work from Dr DiPersio’s lab showed that leukemic mice that receive donor T cells and go on to develop GVHD show a characteristic migration pattern of the T cells through the body. When the cells gather early in the thymus, the mice develop GVHD. When T cells don’t migrate to the thymus, GVHD doesn’t occur.
In the current study, the patients received a relatively small number of CD34-TK75-enriched T cells, so the researchers were not able to show whether the migration patterns in mice were similar in humans.
However, based on the results of this study, Dr DiPersio and his colleagues are participating in a larger trial in partnership with a company based in Italy. The researchers are planning to include patients from multiple medical centers, and each participant should receive about 50 times more of the CD34-TK75-enriched T cells than were administered in this trial.
Washington University is the only center in the new trial that will be able to perform the imaging studies examining migration patterns of the T cells.


