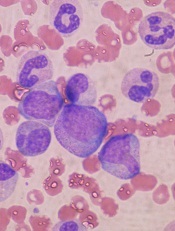
in the bone marrow
New research suggests the cell survival protein MCL-1, a target for a number of new anticancer agents, is essential for hematopoietic recovery.
Investigators found that reducing MCL-1 levels hindered hematopoietic recovery after chemotherapy and radiotherapy caused extensive destruction of mature blood cells.
Reducing MCL-1 also impaired reconstitution of the bone marrow after hematopoietic stem cell transplant (HSCT).
“Our previous research has shown that targeting MCL-1 could be used with great success for treating certain blood cancers,” said Alex Delbridge, PhD, of the Walter and Eliza Hall Institute of Medical Research in Melbourne, Victoria, Australia.
“However, we have now shown that MCL-1 is also critical for emergency recovery of the blood cell system after cancer therapy-induced blood cell loss.”
Dr Delbridge and his colleagues reported these findings in Blood.
Experiments in mice revealed that loss of a single MCL-1 allele, which reduced MCL-1 protein levels, greatly compromised the immune system and hindered red blood cell recovery after treatment with 5-fluorouracil, γ-irradiation, or HSCT.
Further investigation showed that the pro-apoptotic gene PUMA plays a key role in this phenomenon, as MCL-1 inhibits PUMA. In mice, knocking out PUMA alleviated—but did not eliminate—the HSC survival defect caused by deletion of both MCL-1 alleles.
“This exquisite dependency on MCL-1 for emergency blood cell production has important implications for potential cancer treatments involving MCL-1 inhibitors,” Dr Delbridge said.
“If MCL-1 inhibitors are to be used in combination with other cancer therapies, careful monitoring of the blood cell system will be needed,” added Stephanie Grabow, PhD, also of the Walter and Eliza Hall Institute.
“Our institute colleagues are working to evaluate a potential new drug to treat blood cancers by targeting MCL-1. Our findings suggest that MCL-1 inhibitors and chemotherapeutic drugs should not be used simultaneously.”
Dr Delbridge said this research also offers insights that could help improve HSCT.
“Stem cell transplants can be dangerous because, until the blood cell system is functionally restored, patients are vulnerable to infection,” he said. “Our research suggests that increasing levels of MCL-1 or decreasing the activity of opposing proteins could be a viable strategy for speeding up the regeneration process and reducing the risk of infection after stem cell transplantation.”


