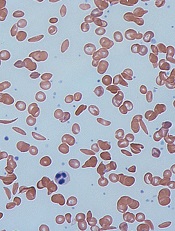
Image by Graham Beards
Results of a small study suggest there may be a high prevalence of sleep disordered breathing (SDB) in adults with sickle cell disease (SCD).
Of the 32 patients included in the study, 44% had a clinical diagnosis of SDB.
These patients had significantly increased REM latency, a significantly higher mean score on the Epworth Sleepiness Scale, and a significantly higher oxygen desaturation index (ODI) than patients who did not have SDB.
However, there was no significant difference between SDB and non-SDB patients with regard to insomnia, delayed sleep phase syndrome, nocturia, or SCD complications.
Sunil Sharma, MD, of Sidney Kimmel Medical College at Thomas Jefferson University in Philadelphia, Pennsylvania, and his colleagues recounted these results in the Journal of Clinical Sleep Medicine.
“Previous research identified pain and sleep disturbance as 2 common symptoms of adult sickle cell disorder,” Dr Sharma said. “We wanted to examine the reasons for the sleep disturbances, as it can have a strong impact on our patients’ quality of life and overall health. We discovered a high incidence of sleep disordered breathing in patients with sickle cell disease who also report trouble with sleep.”
Dr Sharma and his colleagues analyzed 32 consecutive adult SCD patients who had reported symptoms suggesting disordered sleep or had an Epworth Sleepiness Scale score of 10 or greater. The patients underwent a comprehensive sleep evaluation and overnight polysomnography in an accredited sleep center.
SDB was defined as having an apnea-hypopnea index (AHI, events/hour) of 5 or greater. SDB was considered mild if the AHI was 5 to < 15, moderate if the AHI was 15 to < 30, and severe if the AHI was ≥ 30. Once they determined which patients had SDB, the researchers compared these patients to those without the condition.
The team found that 44% of patients (n=14) had SDB. It was mild in 8 patients, moderate in 4, and severe in 2.
Compared to non-SDB patients, those with SDB had a significantly higher mean AHI (1.6 and 17, respectively; P=0.0001), a significantly increased REM latency (98 and 159 minutes, respectively; P=0.014), and a significantly higher mean score on the Epworth Sleepiness Scale (8.6 and 13, respectively; P=0.017).
Patients with SDB also had a significantly higher ODI than non-SDB patients (13 and 1.6, respectively; P=0.0009). Significant oxygen desaturation was defined as oxygen saturation < 89% for 5 cumulative minutes or more. The ODI was the number of recorded oxygen desaturations ≥ 4% per hour of sleep.
There was no significant difference between SDB and non-SDB patients in the incidence of nocturia (2.3 and 1.6, respectively; P=0.063), insomnia (57% and 72%, respectively; P=0.46), or delayed sleep phase syndrome (57% and 50%, respectively; P=0.73).
Delayed sleep phase syndrome was defined as a delay in sleep onset of 2 hours or greater from the desired sleep time and an inability to awaken at the desired time. Insomnia was defined as difficulty initiating sleep (sleep latency greater than 60 minutes) or difficulty maintaining sleep (more than 2 awakenings requiring more than 20 minutes to fall back asleep) on the majority of nights for more than 4 weeks.
There was no significant difference between SDB and non-SDB patients with regard to SCD complications, including crises during sleep (44% and 39%, respectively; P=0.67), average hospital admissions in the last 5 years (9.1 and 6.0, respectively; P=0.15), or average mini-crises per month (2.7 and 3.6, respectively; P=0.69).
Dr Sharma said the diagnosis of SDB could be missed in adults with SCD because they are not generally obese, a common risk factor for SDB, and daytime sleepiness is attributed to the pain medications used to treat the symptoms of SCD. He hopes this study will increase awareness among physicians who can screen patients for SDB.
“Our study suggests that patients with sickle cell disorder should be screened using a questionnaire to identify problems with sleep,” Dr Sharma said. “For further testing, an oxygen desaturation index is another low-cost screening tool that can identify sleep disordered breathing in this population.”


