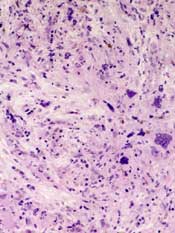
myelofibrosis
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:"Table Normal";
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:"";
mso-padding-alt:0in 5.4pt 0in 5.4pt;
mso-para-margin-top:0in;
mso-para-margin-right:0in;
mso-para-margin-bottom:8.0pt;
mso-para-margin-left:0in;
line-height:107%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:"Calibri","sans-serif";
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;}
Results of a phase 2 study suggest the JAK2/FLT3 inhibitor pacritinib is a feasible treatment option for patients with myelofibrosis who cannot receive or do not respond well to standard therapies.
The drug reduced patients’ spleen volume and improved disease-related symptoms without causing clinically significant myelosuppression.
And pacritinib was considered well-tolerated, even in patients with disease-related anemia and thrombocytopenia.
“Currently, myelofibrosis patients with anemia and thrombocytopenia have limited treatment options for splenomegaly and constitutional symptoms, and
these data show that pacritinib has potential to help patients that are sub-optimally managed on currently available treatments,” said study author Rami S. Komrokji, MD, of the Moffitt Cancer Center in Tampa, Florida.
Dr Komrokji and his colleagues reported these results in Blood. The study was sponsored by CTI Biopharma, the company developing pacritinib.
The researchers evaluated the safety and efficacy of pacritinib in myelofibrosis patients who had clinical splenomegaly that was poorly controlled with standard therapies or who were newly diagnosed with intermediate- or high-risk disease and not considered candidates for standard therapy.
Patients were allowed to enroll irrespective of their degree of thrombocytopenia or anemia. At study entry, 40% of patients had hemoglobin levels below 10 g/dL, and 43% had platelet counts less than 100,000/µL.
A total of 35 patients were enrolled and treated with pacritinib administered at 400 mg once daily in 28-day cycles. The patients’ median age was 69 years.
The primary endpoint was assessment of the spleen response rate, defined as the proportion of subjects achieving 35% or greater reduction in spleen volume from baseline up to week 24, measured by MRI or CT.
A secondary endpoint was the proportion of patients with a 50% or greater reduction in spleen size as determined by physical exam.
The researchers also assessed the proportion of patients with a 50% or greater reduction in total symptom score, which included symptoms of abdominal pain,
bone pain, early satiety, fatigue, inactivity, night sweats, and pruritus, from baseline up to week 24.
Results showed that 30.8% of the evaluable patients (8/26) had a 35% or greater reduction in spleen volume by CT or MRI scan, with 42% of patients reaching a
35% or greater reduction by the end of treatment.
In addition, 42.4% of evaluable patients (14/33) achieved a 50% or greater reduction in spleen size by physical exam. And 48.4% of evaluable patients (15/31) achieved a 50% or greater reduction in total symptom score.
The most common treatment-emergent adverse events were grade 1-2 diarrhea (69%) and nausea (49%). Anemia and thrombocytopenia adverse events were reported in 12 (34.3%) and 8 (22.9%) patients, respectively.
Nine patients (26%) stopped taking pacritinib due to adverse events, but 3 of the events were deemed unrelated to the drug.
There were 5 deaths, 3 of which were due to serious adverse events. Of those, 1 (subdural hematoma) was considered possibly related to pacritinib treatment.


