The US Food and Drug Administration (FDA) has granted fast track designation for CPX-351, a fixed-ratio combination of cytarabine and daunorubicin inside a lipid vesicle, to treat elderly patients with secondary acute myeloid leukemia (AML).
In a phase 2 study of elderly AML patients, there was no significant difference in response or survival rates between patients who received CPX-351 and those who received cytarabine and daunorubicin.
However, CPX-351 conferred a significant response benefit among patients with poor cytogenetics and a significant survival benefit in patients with secondary AML.
“We are pleased that FDA has granted fast track status for CPX-351 for the treatment of elderly patients with secondary AML,” said Scott Jackson, Chief Executive Officer of Celator Pharmaceuticals, the company developing CPX-351.
“Our ongoing phase 3 study in these patients has completed enrollment, and we expect induction response rate data to be available in the second quarter of this year, and to have overall survival data, the primary endpoint of the study, in the first quarter of 2016.”
“If our phase 3 study comparing CPX-351 to the current standard of care is successful, the fast track designation may provide an added benefit of facilitating the [new drug application] review process.”
The FDA established the fast track designation process to expedite the review of drugs that are intended to treat serious or life-threatening conditions and that demonstrate the potential to address unmet medical needs.
The designation allows a drug’s developer to submit sections of a new drug application (NDA) on a rolling basis, so the FDA can review portions of the NDA as they are received instead of waiting for the entire NDA submission. A fast-track-designated product could be eligible for priority review if supported by clinical data at the time of NDA submission.
Phase 2 trial
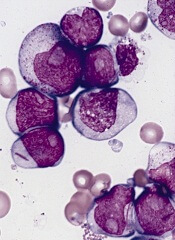
In an article published in Blood last April, researchers reported results with CPX-351 in elderly patients with newly diagnosed AML. The study enrolled 126 patients who were 60 to 75 years of age.
They were randomized to receive CPX-351 (n=85) or “control” treatment consisting of cytarabine and daunorubicin (n=41). The treatment groups were well-balanced for disease and patient characteristics at baseline.
Overall, the response rate was 66.7% in the CPX-351 arm and 51.2% in the control arm (P=0.07). Among patients with adverse cytogenetics, the response rates were 77.3% and 38.5%, respectively (P=0.03). And among patients with secondary AML, response rates were 57.6% and 31.6%, respectively (P=0.06).
The median overall survival was 14.7 months in the CPX-351 arm and 12.9 months in the control arm. The median event-free survival was 6.5 months and 2.0 months, respectively. These differences were not statistically significant.
However, secondary AML patients treated with CPX-351 had significantly better overall survival than secondary AML patients in the control arm. The median overall survival was 12.1 months and 6.1 months, respectively (P=0.01). The median event-free survival was 4.5 months and 1.3 months, respectively (P=0.08).
Common adverse events included febrile neutropenia, infection, rash, diarrhea, nausea, edema, and constipation. There were minimal differences between the treatment arms in the incidence of these events.
The median time to neutrophil recovery was longer in the CPX-351 arm than in the control arm—36 days and 32 days, respectively. And the same was true for platelet recovery—37 days and 28 days, respectively.
Patients in the CPX-351 arm had a higher incidence of grade 3-4 infection than controls—70.6% and 43.9%, respectively—but not infection-related deaths—3.5% and 7.3%, respectively.
By day 60, 4.7% of patients in the CPX-351 arm and 14.6% of patients in the control arm had died. All of these deaths occurred in high-risk patients, particularly those with secondary AML.


