Researchers have found the fusion protein APG101 can rescue erythropoiesis in bone marrow samples from patients with lower-risk myelodysplastic syndromes (MDS).
Previous research suggested that CD95—a receptor that can induce apoptosis when triggered by the CD95 ligand—is overexpressed in two-thirds of patients with lower-risk MDS, and overexpression of CD95 is predictive of a lower response to erythropoiesis-stimulating agents (ESAs).
APG101, which consists of the extracellular domain of the CD95 receptor and the Fc domain of an IgG antibody, is designed to block the CD95 ligand.
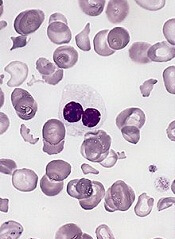
The new study showed that APG101 can inhibit apoptosis in erythrocyte precursor cells and improve their overall proliferation rate. The drug increased the number of burst-forming unit-erythroid (BFU-E) progenitors in samples from MDS patients with low BFU-E numbers at baseline.
“APG101 added to cellular assays efficiently rescued the growth of erythroid progenitors in MDS patients harboring a profound defect of erythropoiesis, independent of the expression level of CD95 or CD95 ligand,” said Michaela Fontenay, MD, PhD, of the Institut Cochin in Paris, France.
Dr Fontenay and her colleagues described these results in Oncotarget. The research was funded by Apogenix, the company developing APG101.
By comparing bone marrow samples from MDS patients and healthy control subjects, the researchers found that CD95, but not CD95 ligand, was overexpressed in patients with lower-risk MDS.
Further analysis revealed that a patient’s CD95 expression level at diagnosis could predict response to an ESA. Specifically, CD95 overexpression was predictive of a lower response rate to ESAs in patients with low- or intermediate-1-risk MDS.
Next, the researchers tested bone marrow erythroid progenitors from 3 control subjects and 5 patients with MDS and found that CD95 expression increased during MDS erythroid progenitor amplification but remained lower in control cultures.
On day 5 of culture, the mean number of BFU-Es was significantly lower in MDS patient samples than in controls. And treatment with APG101 prompted a dose-dependent increase in BFU-E growth in MDS samples but not in controls.
When the researchers added APG101 (at 10 μg/mL) to the cultures over 7 days, they observed an improvement in the proliferation of erythroblasts but no significant effect on the kinetics of differentiation.
They also found that APG101 reduced apoptosis in immature precursors by 30% but had no effect on apoptosis in mature precursors.
Baseline BFU-E number affects response
The researchers then assessed the effects of APG101 in samples from 5 control subjects and 20 MDS patients with varying responses to ESAs and varying baseline levels of BFU-Es.
Fifteen of the MDS patients had a significantly lower number of baseline BFU-Es than controls (P=0.005), but 5 MDS patients had a mean number of BFU-Es that was comparable to controls (P=0.429). There was no significant difference in WHO classification or CD95 expression between the 2 groups of MDS patients (P=0.612).
However, 11 of the 15 patients with low erythropoiesis had received an ESA, and all of them were resistant to this treatment. In all, 15 of the MDS patients had received an ESA, and 14 were resistant to it (6 primary and 8 secondary).
The researchers found that APG101 induced a dose-dependent increase of BFU-Es in samples from the 15 MDS patients with low erythropoiesis but not in samples from the 5 patients with normal erythropoiesis or in the control samples (P<0.001).
The team said that a low BFU-E number at baseline was significantly associated with in vitro response to APG101 among the 20 MDS patients (P=0.031) and the 14 ESA-resistant patients (P=0.027).
Further investigation confirmed that a low clonogenic progenitor number at baseline, but not the level of CD95 or CD95 ligand expression, was predictive of the response to APG101.
“This study provides a rationale for further clinical investigation of this potential new therapeutic option in patients with severely impaired erythropoiesis who are resistant to erythropoiesis-stimulating agents,” Dr Fontenay said.
Apogenix has conducted a phase 1 trial of APG101 in transfusion-dependent patients with low- to intermediate-1-risk MDS. The company expects the results of this trial will be available in the coming months.


