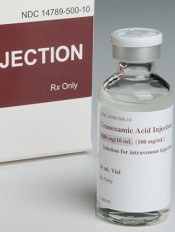
Photo courtesy of NIH
ORLANDO, FL—Results of a large, retrospective study suggest tranexamic acid (TXA) can reduce the need for transfusion in patients undergoing hip and knee replacement surgery without increasing the overall risk of venous thromboembolism (VTE).
However, patients treated with TXA were significantly more likely to develop deep vein thrombosis (DVT) than patients who did not receive the drug.
There was no significant difference between the treatment groups with regard to pulmonary embolism (PE).
These results were presented at the American Academy of Orthopaedic Surgeons (AAOS) 2016 Annual Meeting (abstract P101).
“[C]onflicting results have been published regarding the use of TXA in patients undergoing hip and knee replacement,” said study investigator Geoffrey Westrich, MD, of the Hospital for Special Surgery in New York, New York.
To assess the safety and efficacy of TXA in this patient population, Dr Westrich and his colleagues retrospectively reviewed the records of 4449 patients who had hip or knee replacement over a 6-month period.
There were 720 patients who received TXA topically, 636 who received TXA intravenously, and 3093 patients who did not receive the drug.
The investigators found that 9.7% of patients treated with either type of TXA received a blood transfusion, as did 22.1% of patients who were not treated with TXA.
TXA-treated patients received an average of 0.13 units of blood, compared to 0.37 units for patients in the non-TXA group.
The investigators said there was no significant difference in efficacy between topical and intravenous TXA.
“At our institution, TXA in either intravenous or topical form was effective in decreasing the amount of blood transfusions, as well as the number of units of blood transfused in primary and revision hip and knee replacement,” Dr Westrich said.
“Furthermore, when safety was evaluated, there was no statistically significant difference in blood clots in patients who received IV or topical TXA, reconfirming its safety.”
The odds of developing a hospital-acquired VTE was 1.63 among patients treated with TXA, which was not significantly higher than the odds for patients who did not receive the drug (P=0.24).
When the investigators evaluated DVT and PE separately, they found the TXA group had a significant increase in DVT (P=0.03) but not PE (P=0.94).


