The European Medicines Agency’s Committee for Orphan Medicinal Products (COMP) is recommending orphan designation for the second-generation BTK inhibitor acalabrutinib (ACP-196) for 3 indications.
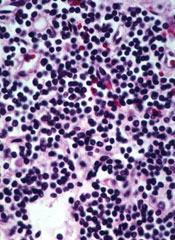
The COMP is recommending the drug receive orphan designation as a treatment for chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), mantle cell lymphoma, and Waldenström’s macroglobulinemia.
The COMP adopts an opinion on orphan drug designation, and that opinion is submitted to the European Commission (EC) for endorsement.
To be granted orphan designation by the EC, a medicine must be intended for the treatment, prevention, or diagnosis of a disease that is life-threatening and has a prevalence of up to 5 in 10,000 in the European Union. Additionally, the medicine must aim to provide significant benefit to those affected by the condition.
Orphan designation provides companies with development and market exclusivity incentives for designated compounds and medicines.
About acalabrutinib
Acalabrutinib is under development by AstraZeneca and Acerta Pharma BV. The drug is currently being evaluated in trials of patients with CLL/SLL, mantle cell lymphoma, Waldentröm’s macroglobulinemia, and a range of other hematologic malignancies and solid tumor cancers.
Data from a phase 1/2 trial of acalabrutinib in CLL were presented at the 2015 ASH Annual Meeting and simultaneously published in NEJM.
The researchers reported on 61 patients with relapsed CLL who had a median age of 62 (range, 44-84) and a median of 3 prior therapies (range, 1-13).
Patients enrolled in the phase 1 portion of the study received escalating doses of acalabrutinib, with a maximum dose of 400 mg once daily. Patients involved in the phase 2 portion of the study were treated with a 100 mg dose twice daily.
At a median follow-up of 14.3 months (range, 0.5 to 20), 53 patients were still receiving treatment.
The most common adverse events of all grades (occurring in at least 20% of patients) were headache (43%), diarrhea (39%), increased weight (26%), pyrexia (23%), upper respiratory tract infection (23%), fatigue (21%), peripheral edema (21%), hypertension (20%), and nausea (20%).
Grade 3/4 adverse events included diarrhea (2%), increased weight (2%), pyrexia (3%), fatigue (3%), hypertension (7%), and arthralgia (2%).
The overall response rate among the 60 evaluable patients was 95%. This included partial responses in 85% of patients and partial responses with lymphocytosis in 10%. The rate of stable disease was 5%.
The researchers noted that responses occurred in all dosing cohorts, and the response rate increased over time.


