A new device might help physicians choose the optimal treatment for cancer patients, according to research published in Nature Biotechnology.
The device was designed to predict responses to treatment by measuring individual cell growth after drug exposure.
Researchers found they could predict whether a particular drug would kill leukemia or glioblastoma cells, based on how the drug affected the cells’ mass.
“We’ve developed a functional assay that can measure drug response of individual cells while maintaining viability for downstream analysis such as sequencing,” said study author Scott Manalis, PhD, of the Massachusetts Institute of Technology in Cambridge.
He and his colleagues were inspired to develop their assay, in part, by a test that has been used for decades to choose antibiotics to treat bacterial infections. The antibiotic susceptibility test involves simply taking bacteria from a patient, exposing them to a range of antibiotics, and observing whether the bacteria grow or die.
To translate that approach to cancer, the researchers needed a way to rapidly measure cell responses to drugs, and to do it with a limited number of cells.
For the past several years, Dr Manalis’s lab has been developing a device known as a suspended microchannel resonator (SMR).
According to the researchers, the SMR can measure cell masses 10 to 100 times more accurately than any other technique. This allows for the precise calculation of growth rates of single cells over short periods of time.
For this study, Dr Manalis and his colleagues used the SMR to determine whether drug susceptibility could be predicted by measuring cancer cell growth rates following drug exposure.
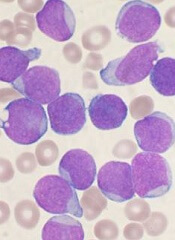
The team analyzed cells from patients with different subtypes of glioblastoma and B-cell acute lymphocytic leukemia (ALL) that have previously been shown to be either sensitive or resistant to specific therapies—MDM2 inhibitors for glioblastoma and BCR-ABL inhibitors for ALL.
After exposing the cancer cells to the drugs, the researchers waited about 15 hours, then measured the cell’s growth rates. Each cell was measured several times over a period of 15 to 20 minutes, providing enough data for the team to calculate the mass accumulation rate.
They found that cells known to be susceptible to a given therapy changed the way they accumulate mass, whereas resistant cells continued to grow as if unaffected.
“We’re able to show that cells we know are sensitive to therapy respond by dramatically reducing their growth rate relative to cells that are resistant,” said study author Mark Stevens, of the Dana-Farber Cancer Institute in Boston, Massachusetts.
“And because the cells are still alive, we have the opportunity to study the same cells following our measurement.”
The researchers said a major advantage of this technique is that it can be done with very small numbers of cells. In the experiments with ALL cells, the team showed they could get accurate results with a droplet of blood containing about 1000 ALL cells.
Another advantage is the speed at which small changes in cell mass can be measured, said Anthony Letai, MD, PhD, of the Dana-Farber Cancer Institute.
“This system is well suited to making rapid measurements,” said Dr Letai, who was not involved in this study. “I look forward to seeing them apply this to many more cancers and many more drugs.”
The researchers are now using their technique to test cells’ susceptibility to drugs, then isolate the cells and sequence the RNA found in them, revealing which genes are turned on.
“Now that we have a way to identify cells that are not responding to a given therapy, we are excited about isolating these cells and analyzing them to understand mechanisms of resistance,” Dr Manalis said.
In another recent paper published in Nature Biotechnology, the researchers described a higher throughput version of the SMR device that can do in 1 day the same number of measurements that took several months with the device used in this study.
This is an important step toward making the approach suitable for clinical samples, Dr Manalis said.


