A decade of follow-up data suggest that patients with newly diagnosed follicular lymphoma may derive long-term benefit from first-line therapy with the R-CHOP regimen, according to investigators in Japan.
Among patients with untreated follicular and other indolent B-cell lymphomas enrolled in a randomized phase 2/3 trial, the 10-year progression-free survival (PFS) rate for patients assigned to R-CHOP-21 (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone every 3 weeks) was 33%, and the 10-year PFS rate for patients assigned to R-CHOP-14 (R-CHOP every 2 weeks with granulocyte colony-stimulating factor [G-CSF] support] was 39%, and these PFS rates did not differ between the treatment arms, Takashi Watanabe, MD, PhD, from Mie University in Tsu, Japan, and his colleagues reported in the Lancet Haematology.
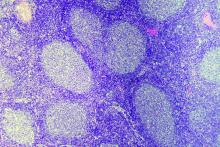
They also found that, compared with therapeutic regimens prior to the introduction of rituximab, R-CHOP was associated with a reduced likelihood of histological transformation of follicular lymphoma into a poor-prognosis diffuse large B-cell lymphoma (DLBCL), with no apparent increase in risk of secondary malignancies.
“The gold-standard, first-line treatment in patients with advanced-stage follicular lymphoma remains undetermined. However, because of the reduction in incidence of transformation without an increase in either secondary malignancies or fatal infectious events, the R-CHOP regimen should be a candidate for standard treatment, particularly from the viewpoint of long-term follow-up,” the investigators wrote
The JCOG0203 trial, which began enrollment in September 2002, included patients with stage III or IV indolent B-cell lymphomas, including grades 1-3 follicular lymphoma, from 44 Japanese hospitals. The patients were randomly assigned to receive six cycles of either R-CHOP-14 plus G-CSF or R-CHOP-21 administered once daily for 6 days beginning on day 8 of every cycle). Patients did not receive rituximab maintenance in either group.
In the primary analysis of the trial, published in 2011, the investigators reported that in 299 patients there were no significant differences in either PFS or 6-year overall survival (OS).
In the current analysis, the investigators reported that, for 248 patients with grade 1-3a follicular lymphoma, the 8-year PFS rate was 39% and the 10-year PFS rate was 36%.
The cumulative incidence of histological transformation was 3.2% at 5 years, 8.5% at 8 years, and 9.3% 10 years after the last patient was enrolled.
“In our study, survival after histological transformation was still poor; therefore, reducing histological transformation remains a crucial issue for patients with follicular lymphoma,” the investigators wrote.
The cumulative incidence of secondary malignancies at 10 years was 8.1%, and the cumulative incidence of hematological secondary malignancies was 2.9%.
The investigators noted that the actual incidence of secondary solid tumors or hematologic malignancies apart from the setting of autologous stem cell transplants is not known and emphasized that patients should be followed beyond 10 years to ensure that the risk of secondary malignancies is not underestimated.
“Clinicians choosing a first-line treatment for patients with follicular lymphoma should be cautious of secondary malignancies caused by immunochemotherapy and severe complications of infectious diseases in the long-term follow-up – both of which could lead to death,” they advised.
The study was supported by the Ministry of Health, Labour and Welfare of Japan and by the National Cancer Center Research and Development Fund of Japan. Dr. Watanabe has received honoraria from Bristol-Myers Squibb, Takeda, Taisho Toyama, Celgene, Nippon Shinyaku, and Novartis and funding resources from TakaraBio and United Immunity to support the Department of Immuno-Gene Therapy at Mie University. Multiple coauthors reported similar relationships.
SOURCE: Watanabe T et al. Lancet Haematol. 2018 Nov;5(11):e520-31.