Care of the cancer patient is complex and expensive. During 2001-2011, medical spending to treat cancer increased from $56.8 billion to $88.3 billion in the United States. During this time, ambulatory expenditures for care and treatment increased while inpatient hospital expenditures decreased.1,2 Treatments for cancer have advanced, but costs do not correlate with outcomes. Advanced payment models aimed at ensuring high quality while lowering costs may be the vehicle to help mitigate the financial burden of cancer treatment on patients and society at large.
Oncology Care Model
The Center for Medicare and Medicaid Innovation designed the Oncology Care Model (OCM), which allows practices and payers in the United States to partner with the Centers for Medicare & Medicaid Services. The goal of the OCM is to provide high quality, highly coordinated cancer care at the same or lower cost. Practice partnerships with the CMS involve payment arrangements that include financial and performance accountability for episodes of cancer care surrounding chemotherapy delivery to patients.3
Practices that have been selected by the CMS have attested to providing a number of enhanced services from 24/7 patient access to an appropriate clinician who can access medical records to having a documented care plan for every patient.4
Payment methodology
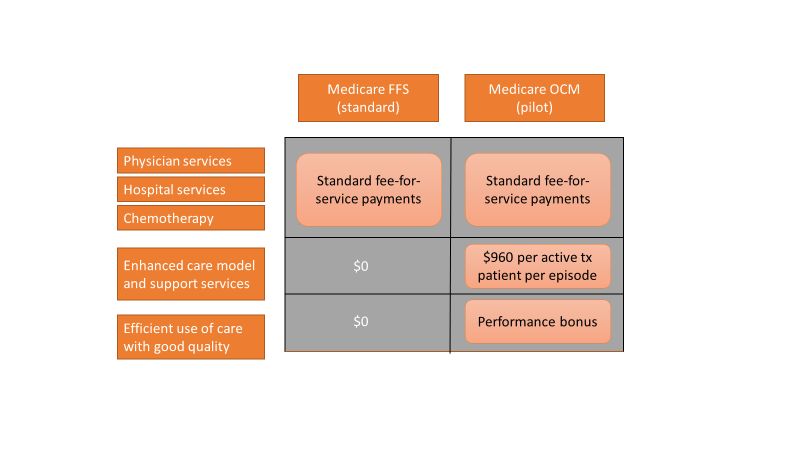
An episode of care is defined as a 6-month period that starts at the time of chemotherapy administration. In addition to the standard fee-for-service payment, practices have the ability to earn two other types of payments during an oncology episode.
The per-beneficiary Monthly Enhanced Oncology Services payment is $960 for the entire episode but is paid to practices at $160 per month.
Practices have the potential to earn additional performance-based payments (PBP) based on the difference in cost between the projected and actual cost of the episode. The PBP also incorporates performance on quality metrics, based on Medicare claims and other information submitted by the practice. For example, claims-based measures include hospital, emergency department (ED), and hospice utilization.
To participate in the OCM, practices must choose either a one-sided or two-sided risk model. In the one-sided risk model, practices take on no downside risk but need to achieve a greater reduction in expenditures (4% below the benchmark price). In the two-side risk model, practices need only to reduce expenditures by 2.75% below the benchmark price. But if they fail to meet their savings goals, they must pay the difference to the CMS. The recoupment is capped at 20% of the benchmark amount.
Feedback reports
The CMS sends quarterly feedback reports that contain information on practice demographics, outcomes, expenditures, chemotherapy use, and patient satisfaction. The outcomes include the mortality rate for Medicare beneficiaries treated at the practice, compared with other practices nationally. In addition, the reports include end-of-life metrics and patient satisfaction, as well as details of expenditures on drugs, hospital use, imaging and laboratory services, and a description of chemotherapy usage.