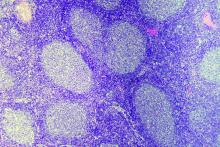
A molecular analysis of a patient with follicular lymphoma (FL) that became B-lymphoblastic leukemia/lymphoma (B-ALL/LBL) uncovered genetic changes that may improve understanding of this transformation.
“The study provides new insights into the pathogenesis of FL-B-ALL/LBL transformation and suggests novel, disease biology–based therapeutic approaches to this aggressive and currently incurable disease,” wrote Jonathan Belman, MD, PhD, of the Hospital of the University of Pennsylvania, Philadelphia, and coauthors. Their findings were published in Cold Spring Harbor Molecular Case Studies.
To further understand the rare occasions when FL transforms into a more aggressive form of lymphoma, the researchers investigated a 36-year-old man with low-grade FL that became B-ALL/LBL roughly 1 year after diagnosis. Their analysis included immunoglobulin (Ig) gene rearrangement studies, cytogenetic analysis, and whole exome sequencing of the patient’s FL, B-ALL/LBL, and normal cells.
Next generation sequencing of Ig rearrangements from normal, FL, and B-ALL/LBL specimens revealed considerable somatic hypermutation (SHM) in a single neoplastic clone – IgHV4-34_JH6 – in the FL cells. By comparison, though no dominant clone was found in the B-ALL/LBL specimen, there was even more extensive SHM, along with clones that could be traced to the FL lineage.
In addition, fluorescence in situ hybridization (FISH) studies on the FL specimen were positive for rearrangements of BCL2 and BCL6 genes; a rearrangement of BCL6 is associated with clinical aggressiveness. Those same two rearrangements were found in the B-ALL/LBL specimen, along with a MYC gene rearrangement unseen in the FL.
“MYC translocations are well known to contribute to high aggressiveness of lymphomas, and are hallmark of FL-B-ALL/LBL transformation,” the researchers wrote.
Finally, comparative whole exome sequencing of normal tissue plus the cancerous specimens identified 751 single nucleotide variants. The normal tissue contained 111 of those mutations, while the FL specimens contained 116 mutations – 11 of which were shared solely with B-ALL/LBL – and the B-ALL/LBL specimens contained a striking 575 unique mutations. Notably, a nonsense mutation in the KMT2D gene that was shared by FL and B-ALL/LBL may have contributed to lymphomagenesis.
The study was funded by a grant from the National Institutes of Health, the Abramson Cancer Center Translational Center in Lymphoma, the Daniel B. Allanoff Foundation, and a Hematopathology Divisional Training grant.
SOURCE: Belman JP et al. Cold Spring Harb Mol Case Stud. 2019 Nov 27. doi: 10.1101/mcs.a004614.