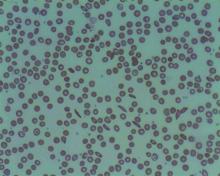
Although a low blood sodium level has been shown to be a prognostic factor for a number of disorders, it has not been reported on for sickle cell disease, according to French researchers Jean-Simon Rech, MD, and colleagues.
They found that hyponatremia at hospital admission was predictive of complications in initially uncomplicated episodes of painful episodes of sickle cell disease (SCD), according to their study published online in the American Journal of Medicine. Dr. Rech is with the department of internal medicine, Sickle Cell Disease Reference Center, Tenon Hospital, Assistance Publique-Hôpitaux de Paris.
The study assessed 1,218 stays (406 patients) admitted to a single center and the analyses were adjusted for age, sex, hemoglobin genotype and concentration, LDH concentration, and white blood cell count.
The researchers found that hyponatremia (defined as plasma sodium ≤ 135 mmol/L) was significantly associated with the primary endpoint of a composite criterion including acute chest syndrome, intensive care unit transfer, red blood cell transfusion, or inpatient death (P = .001).
With regard to the components of the primary endpoint, hyponatremia was significantly associated with acute chest syndrome (P = .008), as well as with receiving a red blood cell transfusion (P < .001) However, hyponatremia at admission was not significantly associated with intensive care unit transfer (P = .074) and there were no patient deaths.
In addition, hyponatremia was significantly associated with longer stays: 1.1 days adjusted mean length of stay (P < .001).
“Hyponatremia may lead to direct clinical consequences in the management of sickle cell disease patients. Indeed, a plasma sodium concentration ≤ 135mmol/L at admission or a decreasing natremia over the first days of an acute painful episode could be regarded as early signs of incipient acute chest syndrome, prompting clinicians to closely monitor the clinical status of their patients,” the researchers concluded.
The authors declared that they had no conflicts and that there was no funding source.
SOURCE: Rech JS et al. Am J Med. 2020 Mar 18. doi.org/10.1016/j.amjmed.2020.02.017.