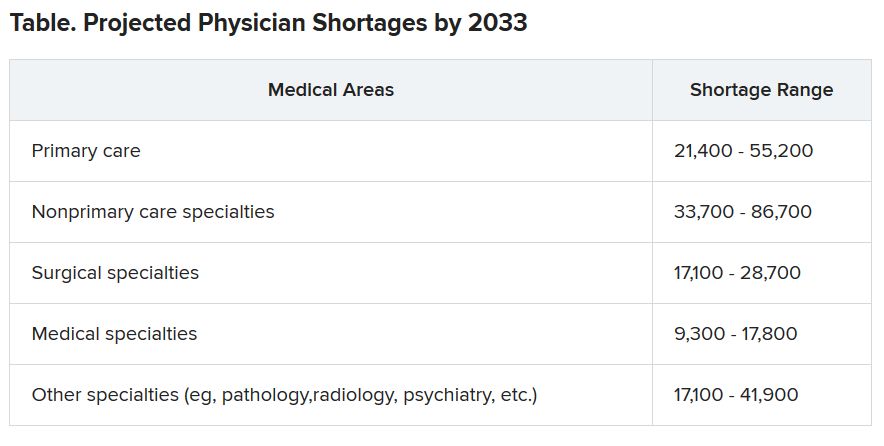
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.