INDIANAPOLIS – Local excision of early invasive stage I colon or rectal carcinoma confers significantly worse 5-year overall and cancer-specific survival than does radical resection, according to analysis of a large national database.
This was true for stage I T1 and T2 disease; that is, for patients with tumor invading the submucosa as well as for those with tumor invading the muscularis propria, Dr. Aneel Bhangu reported at the annual meeting of the American Surgical Association.
In contrast, 5-year survival rates were equivalent with local excision compared with radical resection in patients with stage 0 disease, also known as carcinoma in situ, added Dr. Bhangu of Royal Marsden Hospital, London.
"We recommend that it is safe to perform local excision for stage 0 lesions – that is, carcinoma in situ or severely dysplastic polyps. Refined selection criteria for T1 cancers are required and should be the focus of further research. The use of local excision as a definitive treatment should be carefully considered for patients with T2 colorectal cancer, especially when treating younger, fit patients," he said.
The surgical oncologist presented an analysis of 43,494 patients with surgically treated stage 0 or I adenocarcinoma of the colon or rectum in the Surveillance, Epidemiology, and End Results (SEER) database for 1998-2009. He noted as an aside that the National Cancer Institute’s SEER database is "an open-access and free resource which is the envy of the worldwide oncological community and a shining example of how open-access data can be used by the global community to forward research."
Seventy percent of patients had colonic cancers, 30% rectal. Stage 0 cancer was present in 8.2%, while 91.8% of patients had stage I cancers, 51% of which were T1, 49% T2. Eighteen percent of subjects underwent local excision, while the rest had major resections.
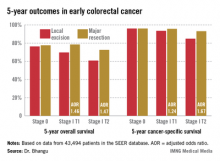
Five-year overall survival was nearly an absolute 8% better in patients with stage I disease treated by radical resection, an advantage that grew even more dramatic in a multivariate analysis adjusted for age and other potential confounders.
Dr. Bhangu observed that these findings take on added import because the number of patients presenting with early colorectal cancer is climbing as a consequence of effective population-based colorectal cancer screening programs. The use of local excision as treatment for such cancers is growing as well. Yet the availability of high-tech tools and techniques for endoscopic local excision of these malignancies has created a dilemma: Such surgery spares the patient from a major operation with all its attendant hazards and morbidity, but when recurrences of these initially small cancers happen they may be inoperable in 10% of cases, and even when they are operable they require extensive visceral resection up to 50% of the time.
Discussant Dr. Genevieve Melton-Meaux of the University of Minnesota, Minneapolis, noted that a surprisingly large percentage of younger patients with stage I disease in this series – that is, patients under age 60 – were treated via local excision.
"We, too, were surprised by this," Dr. Bhangu replied. "If I were to speculate why, I’d say that it may be an issue of clinician equipoise. Some surgeons and endoscopists are true believers in this technology and they may be applying it to a wide scope of patients."
This same lack of equipoise explains the glacially slow recruitment rates into ongoing clinical trials badly needed to establish evidence-based therapy for early-stage colorectal cancer, he added.
He and his coworkers recommended directing future research in this field toward determining which patients with stage I disease are appropriate for local excision. Potentially relevant pathologic markers include depth of invasion and the degree of tumor differentiation. Biomarkers predictive of recurrence also are sorely needed.
Discussant Edward M. Copeland III noted that in light of Dr. Bhangu’s findings it makes sense to offer patients with T2 lesions neoadjuvant radiation and/or chemotherapy.
"You’d probably downstage a lot of them to T0 and you could then locally excise them, doing away with that 8% difference in survival between local excision and major resection you found in the SEER database," said Dr. Copeland, professor and chairman of the department of surgery at the University of Florida, Gainesville.
"I would venture to say if you had a patient with a T2 rectal lesion and offered neoadjuvant therapy followed by local excision, without a major operation, and with virtually zero chance of recurrence, I would take that, personally," he added.
Dr. Bhangu responded that it’s an intriguing notion, but the supporting evidence simply doesn’t exist. However, an ongoing U.K. randomized trial is evaluating just such an approach in patients with stage I T1 and T2 rectal cancer.