SAN FRANCISCO – A 3-minute MRI allowed a radiologist to rule out breast cancer with 99% accuracy in a prospective study of 443 women at a slightly increased or intermediate lifetime risk of breast cancer.
Extending the expert’s reading time to no more than 30 seconds to also interpret the first postcontrast subtracted (FAST) images provided the same sensitivity and specificity as a full diagnostic MRI protocol that had patients on the MRI table for 21 minutes on average, Dr. Christiane K. Kuhl reported at a breast cancer symposium sponsored by the American Society of Clinical Oncology.
Conventional breast MRI protocols are time consuming and more expensive, because they are designed for diagnosis, not screening, said Dr. Kuhl, director of the department of diagnostic and interventional radiology at Rheinisch-Westfälische Technische Hochschule Aachen (Germany) University. The study aimed to trade some of the high sensitivity of MRI in detecting breast cancer for faster image acquisition and interpretation, perhaps eventually leading to lower cost and greater accessibility to MRI.
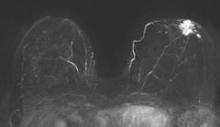
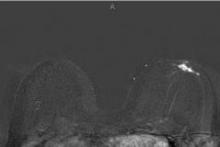
For the study, experienced breast radiologists were asked to review the maximum intensity projection (MIP) of the FAST images to determine whether there was significant enhancement. They then examined the FAST images for possible further categorization of any enhancement seen on the MIP, and analyzed the MRI under the full diagnostic protocol.
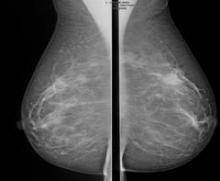
The prospective proof-of-concept study included patients who had imaging done between January 2009 and June 2010 and who were followed for 2 years to validate negative diagnoses. These were asymptomatic women with an intermediate risk with less than a 25% estimated lifetime risk of breast cancer. All of the women had a normal or benign mammogram and, if they had dense breasts, a normal or benign ultrasound result.
Acquiring the MIP and FAST images took less than 3 minutes with the patient on the MRI table. Reading the maximum intensity projection averaged 3 seconds, and reading the MIP plus FAST image averaged 28 seconds.
MRI screening identified 11 cancers, for an additional yield of 18 cancers per 1,000 examinations beyond what could be detected by mammography. Reading the MIP alone had a negative predictive value of 99%; the maximum intensity projection plus FAST readings and the full MRI protocol had negative predictive values just under 100%, Dr. Kuhl reported. The sensitivity of the MIP was close to 95% compared with 100% for MIP plus FAST or the full protocol. The specificity and positive predictive value could not be calculated for the MIP because the MIP reading detected only the presence or absence of significant enhancement. Evaluating the MIP plus FAST or the full MRI protocol produced similar specificities (in the mid-90% range) and positive predictive values (in the low 20% range).
All 11 breast cancers were intermediate- or high-grade cancers; 4 were ductal carcinoma in situ (DCIS) and 7 were invasive cancers. The median tumor size was 8 mm, and the mean age of the women with cancer was 51 years.
Conventional breast cancer screening using mammography picks up cancers that may be prognostically irrelevant, which add to potential overdiagnosis of breast cancer, she noted. In 11 studies that compared screening with breast MRI and mammography, MRI detected two to four times as many cancers as did mammography or ultrasound. Finding more DCIS and invasive cancers via MRI doesn’t necessarily add to the problem of overdiagnosis, she said, because the issue is as much underdiagnosis of prognostically relevant disease as it is overdiagnosis of relevant disease.
The technology of mammography favors detection of slowly growing cancers because of its focus on architectural distortions, spiculations, and calcifications that reflect regressive changes, while MRI technology detects angiogenic and protease activity that is biased toward biologically active disease, she said.
Previous data from her institution show that the sensitivity of MRI for detecting DCIS increases from 80% with low-grade DCIS to 98% with high-grade DCIS, but the sensitivity of mammography decreases as DCIS grade increases, dropping from 61% with low-grade DCIS to 35% with high-grade DCIS without necrosis*.
The symposium was cosponsored by the American Society of Breast Disease, the American Society of Breast Surgeons, the National Consortium of Breast Centers, the Society of Surgical Oncology, and the American Society for Radiation Oncology.