Lack of PPE and fear among health care staff
There have been widespread reports in the media, and several anecdotal reports, about severe shortages of personal protective equipment (PPE), and as a result, an increase in fear and anxiety among frontline health care workers.
In addition, there also have been reports about hospital administrators disciplining medical and nursing staff for voicing their concerns about PPE shortages to the general public and the media. This likely stems from the narrow “optics” and public relations concerns of health care facilities.
It is evident that the size and magnitude of the COVID-19 pandemic was grossly underestimated, and preparations were inadequate. But according to past surveys of health care workers, a good number of them believe that medical and nursing staff have a duty to deliver care to sick people even if it exposes them to personal danger.
Given the special skills and privileges that health care professionals possess, they do have a moral and ethical responsibility to take care of sick patients even if a danger to themselves exists. However, society also has a responsibility to provide for the safety of these health care workers by supplying them with appropriate safety gear. Given the unprecedented nature of this pandemic, it is obvious that federal and state governments, public health officials, and hospital administrators (along with health care professionals) are still learning how to appropriately respond to the challenge.
It would be reasonable and appropriate for everyone concerned to understand and acknowledge that there is a shortage of PPE, and while arranging for this to be replenished, undertake and implement measures that maximize the safety of all health care workers. An open forum, mutually agreed-upon policy and procedures, along with mechanisms to address concerns should be formulated.
In addition, health care workers who test positive for COVID-19 can be a source of infection for other health care workers and non-infected patients. Therefore, health care workers have the responsibility of reporting their symptoms, the right to have themselves tested, and they must follow agreed-upon procedures that would limit their ability to infect other people, including mandated absenteeism from work. Every individual has a right to safety at the workplace and this right cannot be compromised, as otherwise this will lead to a suboptimal response to the pandemic. The government, hospital administrators, and health care workers will need to come together and work cohesively.
Ethical issues surrounding resource allocation
At the time of hospital admission, any suspected or confirmed COVID-19 patient should have his or her wishes recorded with the admitting team regarding the goals of care and code status. During any critical illness, goals evolve depending on discussions, reflections of the patient with family, and clinical response to therapy. A patient who does not want any kind of life support obviously should not be offered an ICU level of care.
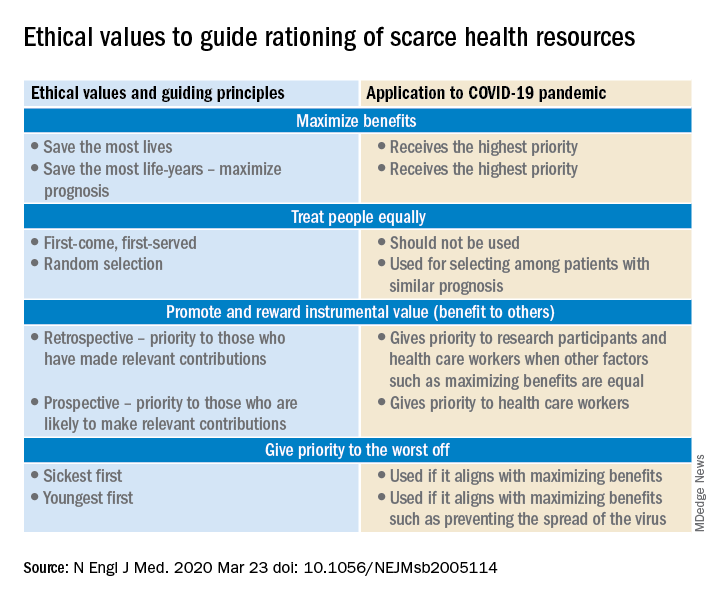
On the other hand, in the event of resources becoming overwhelmed by demand as can be expected during this pandemic, careful ethical considerations will need to be applied.
A carefully crafted transparent ethical framework, with a clear understanding of the decision-making process, that involves all stakeholders – including government entities, public health officials, health care workers, ethics specialists, and members of the community – is essential. Ideally, allocation of resources should be made according to a well-written plan, by a triage team that can include a nontreating physician, bioethicists, legal personnel, and religious representatives. It should not be left to the front-line treating physician, who is unlikely to be trained to make these decisions and who has an ethical responsibility to advocate for the patient under his care.