Schizophrenia spectrum disorder is associated with a significantly increased risk of dying from COVID-19, new research shows.
After adjusting for demographic and medical risk factors, the investigators found that patients who had been diagnosed with schizophrenia were two to three times more likely to die of COVID-19 if they contracted the disease.
“ and efforts should be taken to reduce risk of infection [social distancing, masks, etc.], particularly in people with schizophrenia who live in congregate living situations [hospitals and group residences],” Donald Goff, MD, department of psychiatry, New York University Langone Medical Center, said in an interview.
The study was published online Jan. 27 in JAMA Psychiatry.
The study included 7,348 adults with laboratory-confirmed SARS-CoV-2 infection from the NYU Langone Health System; 75 (1.0%) had a history of schizophrenia spectrum disorder, 564 (7.7%) had a history of a mood disorder, and 360 (4.9%) had a history of an anxiety disorder.
Overall, 864 patients (11.8%) died or were discharged to hospice within 45 days of a positive SARS-CoV-2 test.
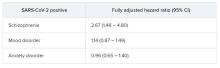
In the fully adjusted model, a premorbid diagnosis of schizophrenia spectrum disorder, but not mood or anxiety disorder, was significantly associated with an increased risk of dying from COVID-19 within 45 days.
”A higher risk with schizophrenia spectrum diagnoses was expected based on previous studies of all-cause mortality, but the magnitude of the increase after adjusting for comorbid medical risk factors was unexpected,” the researchers wrote in the study, first authored by Katlyn Nemani, MD, research assistant professor of psychiatry at NYU Langone.
‘Alarming finding’
In an interview, Luming Li, MD, Yale New Haven (Conn.) Psychiatric Hospital, noted that, although the number patients with schizophrenia spectrum disorders in the sample is “fairly low,” she was not surprised by the increased risk for death from COVID-19.
“Schizophrenia falls into the serious mental illness category, and these patients are more often predisposed to homelessness, comorbid medical and substance use, living in congregate settings, lower socioeconomic status, etc,” Dr. Li noted.
Dr. Li’s advice for clinicians who treat patients who have schizophrenia during the COVID-19 pandemic is to minimize their risk in various care settings through the use of personal protective equipment and other infection prevention techniques.
“If a patient does contract COVID-19, make sure patient’s care is escalated appropriately, given the higher risk for mortality in patients with schizophrenia spectrum disorders,” she said.
Tom Pollak, PhD, MRCPsych, King’s College London, said that it has been known for some time that patients with serious mental illness have poorer physical health outcomes. More recently, it has been shown that those who have been diagnosed with psychiatric disorders appear to be at greater risk for poor COVID-19 outcomes.
“This study is the first to specifically highlight schizophrenia spectrum disorders as being particularly at risk. This is an alarming finding. These patients are already amongst the most vulnerable members of society and are probably underserved by most health care systems worldwide,” Dr. Pollak said in a statement.
“Although these findings need urgent replication in larger samples, there are clear reasons for policymakers to take notice now, including giving immediate consideration for prioritization of patients with serious mental illness in nationwide COVID-19 vaccination programs,” he added.
Matthew Hotopf, PhD, FRCPsych, FMedSci, also with King’s College London, said that the New York group has identified people with severe mental disorders as “a high-risk group, and this has immediate public health implications regarding vaccination – that’s the important message of the paper.
“Schizophrenia and other severe psychiatric disorders are risk factors for mortality in the general population before COVID. This is a group with a 10- to 20-year reduction in life expectancy – more than for many diseases we associated with early death,” said Dr. Hotopf.
“The reasons for this are multifactorial, including social deprivation, lifestyle factors (people with schizophrenia smoke more and have high rates of obesity), harms associated with some medications used to treat psychosis, and differential access to health care,” he noted.
“In COVID, we know that deprivation is associated with a much higher mortality, so we would therefore expect that people with severe mental illness will be particularly disadvantaged,” he said.
The study had no specific funding. Dr. Goff has received research support and travel reimbursement from Avanir Pharmaceuticals and Takeda. Dr. Nemani, Dr. Li, Dr. Pollak, and Dr. Hotopf disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.