The Obama administration has announced a new action plan to combat the rise of multidrug-resistant tuberculosis (MDR-TB).
The plan, published Dec. 22, outlines three primary goals to accomplish between 2016 and 2020: strengthening domestic capacity to treat the disease, improving international ability and collaboration, and accelerating research and treatment of MDR-TB.
To strengthen state and local capacity to prevent transmission of TB, the action plan proposes improving surge capacity for rapid response to individual patients, patient clusters, and larger outbreaks of drug-resistant TB, as well as advancing the treatment of latent TB infection and disease among vulnerable populations.
Disease surveillance will be upgraded to “gather, store, analyze, and report electronic data on drug-resistant TB.” As part of the effort, the Centers for Disease Control and Prevention will increase its capacity to use “whole-genome sequencing to elucidate paths of transmission, identify recent transmission, and identify emerging patterns of resistance,” according to the action plan.
Taken with other preventive activities, the measures are estimated to result in a 15% reduction in newly diagnosed MDR-TB cases by 2020, as specified in the National Action Plan for Combating Antibiotic-Resistant Bacteria.
Additionally, the U.S. government will work with partners including the World Health Organization and the Stop TB Partnership to support countries in developing new approaches to MDR-TB. The focus is expected to initiate treatment for an additional 200,000 people with MDR-TB during 2015-2019; an estimated 360,000 people are currently treated under the U.S. government’s Global TB Strategy. The action plan also aims to improve access to patient-centered diagnostic and treatment services in countries with limited health care resources.
Developing a TB vaccine is a key initiative. The plan details that the National Institutes of Health and the CDC will focus on expanding the dialogue among basic scientists, funders, and vaccine developers to identify strategies for vaccine development and preventive drugs.
The plan also urges focused research into the discovery of biological markers that indicate early response to therapy or protection against TB.
Pulmonologist Daniel R. Ouellette of Henry Ford Hospital in Detroit, said “the three goals are certainly worthy,” but the plan does not address the budgetary measures to be taken to increase domestic capacity to combat TB nor does it explain where resources will be found to encourage the development of new medications.
“How much money are we willing to spend in addition to what we spend now in treating general TB? he asked in an interview. “How are we going to incentivize industry to develop new drugs? It all sounds really good, but all of this is going to cost money. Where are the dollars that go with that?” said Dr. Ouellette, who is chair of the Guideline Oversight Committee for CHEST (the American College of Chest Physicians).
The national action plan states that all activities noted will be subject to budgetary constraints and other approvals, including the “weighing of priorities and available resources by the administration in formulating its annual budget and by Congress in legislating appropriations.”
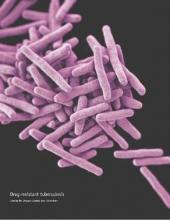
TB causes the deaths of more than 1.5 million people worldwide annually, according to White House data. Nearly one-third of the world’s population is thought to be infected with Mycobacterium tuberculosis; each year, more than 9.5 million develop active TB and about 480,000 people develop MDR-TB. Fewer than 20% with MDR-TB receive appropriate therapy, and less than half are effectively treated.
On Twitter @legal_med