A small number of women reported adverse events related to hypotension and syncope while taking flibanserin and drinking alcohol, an analysis of data from five phase III trials has shown.
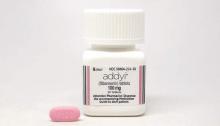
Flibanserin is the first drug approved by the Food and Drug Administration for low female sexual desire in premenopausal women. When the FDA approved flibanserin in August 2015, the agency gave it a boxed warning contraindicating alcohol use with the drug because of a risk of severe hypotension and syncope. The FDA also directed Sprout Pharmaceuticals, who markets the drug as Addyi, to conduct postmarket studies into the relationship between hypotension- and syncope-related events concurrent with alcohol use.
Flibanserin is metabolized through the CYP3A4 system, creating the potential for drug-drug and drug-alcohol interactions. A mixed agonist/antagonist for serotonin and dopamine receptors, flibanserin is taken orally at bedtime on a long-term basis, typically in doses of 100 mg.
Events related to hypotension and syncope include circulatory collapse, hypotension, loss of consciousness, orthostatic hypotension, syncope, vasovagal syncope, and light-headedness.
The industry-funded post hoc analysis included data from five phase III randomized, double-blind placebo-controlled studies of 3,448 premenopausal women. Of the 1,543 taking flibanserin 100 mg at bedtime for up to 24 weeks, 898 reported alcohol use at baseline. Six of these women reported a total of eight adverse events related to hypotension and syncope. In addition, two women who took flibanserin and reported they did not use alcohol had syncope-related events.
Of the 1,905 women taking a placebo, 1,212 reported alcohol use at baseline. Four of these women reported hypotension- and syncope-related adverse events. One woman in the placebo group who reported no alcohol use had two syncope-related adverse events.
Discontinuation rates due to hypotension or syncope among flibanserin users were virtually the same among those who did and did not report alcohol use: 1.8% vs. 1.7%. Among women in the placebo group, those who did not use alcohol had a discontinuation rate of 0.3%, while alcohol users who received placebo had a discontinuation rate of 0.15%.
“It is interesting to note that of the six alcohol users who took flibanserin and had syncopal or hypotensive episodes, four of them continued dosing and completed the study,” Dr. Stuart Apfel, the study’s lead author, said in an interview. “Of the two who did discontinue, one did so because of the syncopal event; the other did so because of somnolence, which is the most common side effect whether one takes alcohol with it or not.”
Dr. Apfel and his colleagues acknowledged that the analysis was limited by the fact that alcohol use was based on self-reports, rather than direct measurement. However, when asked if the drug is safe even if a woman has used alcohol more than she has reported, Dr. Apfel said he personally believes it’s safe, based on the data.
Although there is an increased risk of hypotension and/or syncope with the combination of alcohol use and flibanserin, Dr. Apfel said the risk “appears to be very small, and only moderately higher than [for] those who did not take alcohol.” But the FDA appears to disagree, and after reviewing these same data, required that alcohol use be listed as a contraindication, he added. “I personally don’t think the data indicates that there is a major risk, but it is obviously open to interpretation.”
Dr. Apfel is a consultant to Sprout Pharmaceuticals and Valeant Pharmaceuticals. The studies were supported by Boehringer Ingelheim. Other support was provided by Valeant Pharmaceuticals. The data were presented at the 2016 American Urological Association annual meeting in San Diego.
On Twitter @whitneymcknight