PORTLAND, ORE. – The presence of at least three out of four chemical biomarkers can predict the development of Parkinson’s disease at 3 years of follow-up in people with multiple risk factors for the disease, according to David Goldstein, MD.
These biomarkers, found in the cerebrospinal fluid and in the heart, represent catecholaminergic neurodegeneration.
The PDRisk study of the National Institute of Neurological Disorders and Stroke (NINDS) is investigating whether individuals with at least three out of four statistical risk factors for Parkinson’s disease (PD) develop the disease, based on chemical biomarkers of neurodegeneration. The risk factors are family history of the disease, olfactory dysfunction, dream enactment behavior, and orthostatic hypotension. The biomarkers are PET neuroimaging or cerebrospinal fluid (CSF) neurochemical indicators of catecholamine deficiency in the brain or heart. All the biomarkers are related to dopamine, its precursor, or its metabolites.
In this prospective cohort study, 3,176 individuals supplied risk factor data, of whom 388 reported at least three risk factors. Thirty-one of them had risk factors confirmed and underwent biomarkers testing. The investigators followed 22 of the 31 at approximately 18-month intervals for at least 3 years.Four individuals out of the 22 reached the primary endpoint, which was a diagnosis of PD by a neurologist unaware of the biomarker data. Two of the four individuals with PD also had Lewy body dementia.
“All of the people who went on to convert [to PD], all of them, had at least three of those biomarkers positive. And among the 18 who so far haven’t developed Parkinson’s, none of them had three or more biomarkers. Most of them had none,” said Dr. Goldstein, director of the clinical neurocardiology section at the NINDS. He presented this first look at the PDRisk Study outcome data at the World Parkinson Congress.
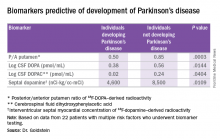
Among 10 healthy control subjects without any risk factors for PD, 1 had two positive biomarkers, and the rest had none. Individuals who converted to PD could be distinguished from those who did not by low values for the posterior/anterior ratio of putamen 18F-DOPA–derived radioactivity, CSF DOPA, CSF 3,4-dihydroxyphenylacetic acid (DOPAC, a metabolite of dopamine), and septal myocardial 18F-dopamine-derived radioactivity. Almost 20 years ago, Dr. Goldstein found that there is a substantial loss of sympathetic noradrenergic nerves in the heart in PD.
He has weighted all the biomarkers as if they had equal contributions, which “is not fair,” he said. All four biomarkers were predictive on their own, but some were more potent than others, notably the ratio of DOPA in the anterior to posterior putamen and low values for DOPA in the CSF. He noted that this finding is the first time CSF DOPA has been documented as a biomarker for the development of PD.
“What that says is that in people who are matched for risk, if you have multiple positive biomarkers, the positive predictive value at 3 years is 100%. And if you have two or fewer biomarkers, the negative predictive value at 3 years is 100%. So that’s why it’s such an astounding set of findings,” he said.The question remains about what to do with these predictors of PD if they are validated. Dr. Goldstein said they could be used to track the efficacy of any intervention to slow the decline to PD.
The study was run by the NINDS and had no outside support. Dr. Goldstein is a U.S. government employee and reported having no financial disclosures.