Stool calprotectin correlates with severity of small-bowel Crohn’s disease, as measured against balloon-assisted enteroscopy and computed tomography enterography, according to a review reported in the January issue of Clinical Gastroenterology and Hepatology of 89 patients at Toho University in Chiba, Japan.
Although the correlation was moderate, the findings suggest that fecal calprotectin (FC), with additional work, might turn out to be a good biomarker for tracking small-bowel Crohn’s disease (CD) and its response to tumor necrosis factor blockers. “Currently, it is not widely accepted that FC relates to disease activity in patients with small-intestinal CD,” said investigators led by Tsunetaka Arai of Toho University’s division of gastroenterology and hepatology (Clin Gastroenterol Hepatol. 2016 Aug 23. doi: 10.1016/j.cgh.2016.08.015).
An FC cutoff of 215 mcg/g identified mucosal healing with 82.8% sensitivity, 71.4% specificity, and an area under the receiver operating characteristic curve of 0.81. Until now, “the most appropriate cutoff value for FC has not been determined to identify a subgroup of patients in clinical remission but with endoscopically active CD or ulcerative colitis,” the Japanese team said.Gastroenterologists need a decent biomarker for small-bowel Crohn’s because old-school endoscopy falls short. Adhesions and strictures block endoscopes, and sometimes scopes simply can’t reach the disease site.
Balloon-assisted enteroscopy (BAE) and computed tomography enterography (CTE) have emerged in recent years as alternatives, but, even so, the need persists for a noninvasive and inexpensive biomarker that’s better than the current standard of C-reactive protein (CRP), which can be thrown off by systemic inflammation, among other problems. The Toho investigators “believe that FC could be a relevant surrogate marker of disease activity in small-bowel CD.” Stool calprotectin paralleled disease activity in their study, while “neither the CDAI [CD activity index] score nor serum CRP showed similar correlation,” they said.
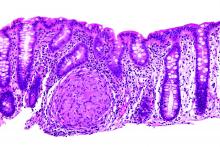
However, elevations in FC – a calcium- and zinc-binding protein released when neutrophils, monocytes, and macrophages inflame the intestinal mucosa – was independent of CD location, which signals the need for further investigation.
Meanwhile, the decent correlation between FC and CTE in the study “should [also] mean that” they could be used together to reliably define mucosal healing. CTE on its own “showed good correlation” with BAE; a CTE score/segment less than 2 [was] associated with endoscopic mucosal healing” on BAE, the investigators said.
The study subjects were an average of 32 years old, and had CD for 9 years; most were men. They had highly active disease at their first endoscopy (average CDAI of 120 points), and an average CRP of 1.09 mg/dL. Twenty-seven patients (30.3%) had small-bowel CD, 50 (56.2%) had ileocolonic CD, and 12 (13.5%) had colonic CD.
They all had endoscopic exams, BAE, and FC stool testing; those with strictures (17) went on to CTE; CTE detected every lesion despite the strictures.
The authors had no conflicts of interest.