LAS VEGAS – Patients with knee osteoarthritis (OA) and a meniscal tear who underwent arthroscopic partial meniscectomy (APM) subsequently experienced accelerated structural progression of their OA, compared with those randomized to physical therapy alone in the randomized METEOR trial.
“In discussing treatment options for symptomatic meniscal tear, patients and providers must weigh the potential benefits and risks of arthroscopic partial meniscectomy, including this increased risk of structural progression,” Jamie E. Collins, PhD, said at the World Congress on Osteoarthritis.
The METEOR (Meniscal Tear in Osteoarthritis Research; NCT00597012) findings are clinically relevant because an estimated 14 million Americans have knee OA, and three-quarters of them also have MRI evidence of a meniscal tear, observed Dr. Collins, a senior statistician at the Orthopaedic and Arthritis Center for Outcomes Research at Brigham and Women’s Hospital, Boston.A thorough physician-patient discussion also needs to mention that several large randomized trials have suggested that patients with meniscal tear and osteoarthritic changes experience similar pain relief with APM plus physical therapy (PT) as compared with PT alone, she added at the congress sponsored by the Osteoarthritis Research Society International.
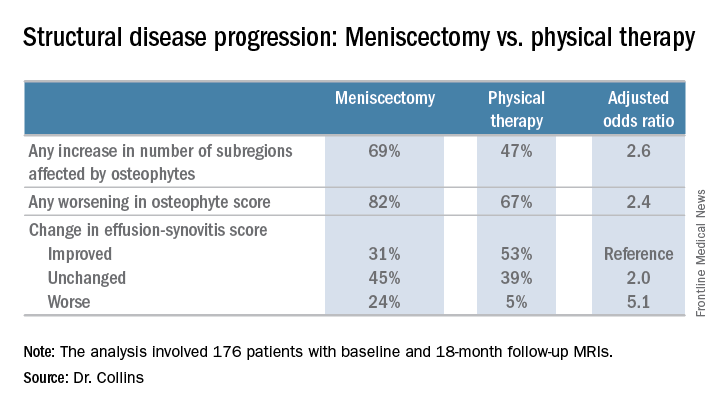
The METEOR trial was a seven-center U.S. randomized trial of APM plus PT or PT alone in patients with MRI or radiographic evidence of OA changes, a meniscal tear on MRI, and mechanical knee symptoms. Dr. Collins reported on 176 randomized patients with baseline and 18-month follow-up MRIs read by a specialist musculoskeletal radiologist. This analysis excluded the 37 patients in the PT group who crossed over to APM within 6 months after randomization.
In an analysis adjusted for baseline Kellgren-Lawrence grade of radiographic knee changes and other potential confounders, the surgically treated group was 2.6 times more likely to demonstrate an increase in the number of knee subregions affected by osteophytes on their MRIs at 18 months. They were also 2.4 times more likely to have any worsening in osteophyte score and 5.1 times more likely to have worsening of their effusion-synovitis score on the MRI OA Knee Score. In addition, the APM group also demonstrated both worsening cartilage thickness and surface area.
There was no significant difference between the two treatment groups in changes in bone marrow lesions or Hoffa-synovitis.
A secondary analysis that incorporated the 37 crossovers from PT to APM within 6 months showed similarly accelerated OA progression after arthroscopic surgery.
“Future work should focus on determining whether this accelerated structural progression is associated with changes in symptoms and ultimately with a higher risk of total knee replacement. In other words, is 2+ structural worsening something that’s noticeable or important for patients?” Dr. Collins concluded.
She reported having no financial conflicts regarding her study, which was sponsored by Brigham and Women’s Hospital.