In the wild world of health care rankings, a year can make a big difference … or not.
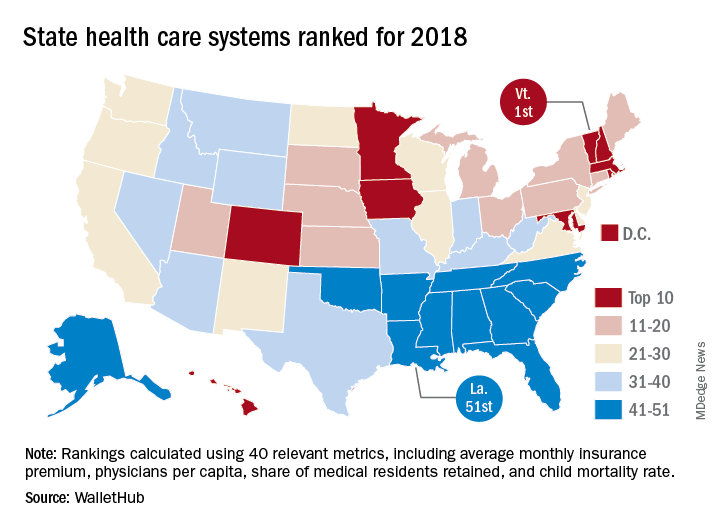
Iowa fell from second to ninth over the course of the last year while Connecticut and South Dakota moved out of the top 10 to make way for Colorado and Maryland, according to WalletHub.
There was less movement at the other end of the rankings, however, with no change at all in the bottom five: Louisiana finished 51st again (the rankings include the District of Columbia), preceded by fellow repeaters Mississippi (50), Alaska (49), Arkansas (48), and North Carolina (47). Texas and Nevada did manage to move on up out of the bottom 11 – to 38th and 40th, respectively – at the expense of Oklahoma and Tennessee, WalletHub reported.
For 2018, the company compared the states and D.C. “across 40 measures of cost, accessibility and outcome,” which is five more measures than last year and a possible explanation for the changes at the top. The cost dimension’s five metrics included cost of medical visits and share of high out-of-pocket medical spending. The accessibility dimension consisted of 21 metrics, including average emergency department wait time and share of insured children. The outcomes dimension included 14 metrics, among them maternal mortality rate and share of adults with type 2 diabetes.
Vermont did well in both the outcomes (first) and cost (third) dimensions but only middle of the pack (23rd) in access. The District of Columbia was ranked first in cost and Maine was the leader in access. The lowest-ranked states in each category were Alaska (cost), Texas (access), and Mississippi (outcomes), according to the WalletHub analysis, which was based on data from such sources as the Centers for Disease Control and Prevention, the Health Resources & Services Administration, and the United Health Foundation.